Not all genetic fusions are created equal. In a new Cancer Discovery study, titled “EML4-ALK variant-specific genetic interactions shape lung tumorigenesis,” scientists from the German Cancer Research Center (DKFZ) and Stanford University reveal that different EML4-ALK fusion variants—the oncogenic drivers behind about 5% of lung adenocarcinomas—behave more like distinct oncogenes. Their findings, uncovered with advanced CRISPR genome editing in mice, could reshape how clinicians classify and treat these tumors.
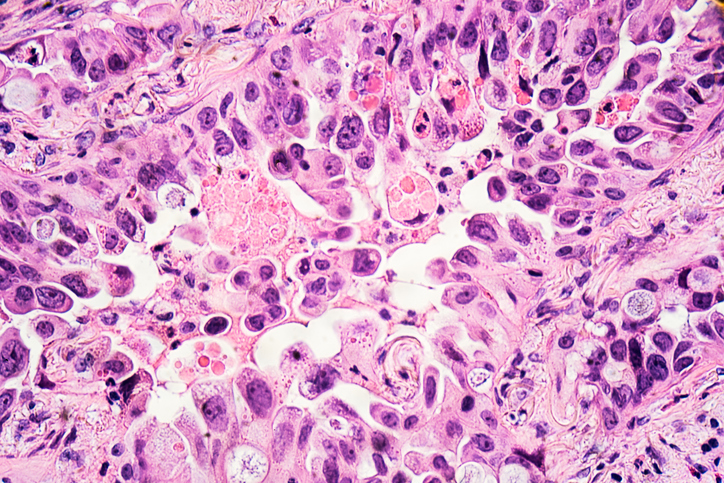
The EML4-ALK fusion occurs when parts of the EML4 and ALK genes break and rejoin, creating an abnormal protein that fuels cancer growth. But the precise breakpoints vary, producing multiple “variants,” or fusion versions, that differ in length and structure. Until now, patients harboring these fusions have typically been grouped together and treated with the same ALK-targeted drugs.
“Until now, all patients with ALK fusions were lumped together and treated with the same drugs,” said senior author Rocío Sotillo, PhD, of DKFZ. “Our research shows that this one-size-fits-all approach overlooks important biological differences.”
To probe these differences, first author Alberto Diaz-Jimenez, PhD, and colleagues used somatic CRISPR/Cas9 genome editing to engineer autochthonous mouse models that recapitulate the two most common human EML4-ALK fusion variants, V1 and V3.
The results were striking. Mice carrying the V3 fusion developed larger tumors more quickly and with a shorter survival time than those with the V1 variant, showing that V3 is intrinsically more oncogenic.
The team next explored how additional genetic factors influence these tumors. They systematically inactivated 29 known or suspected tumor suppressor genes in the V1 and V3 models. They discovered that the impact of many suppressor genes was variant-specific. For example, some tumor suppressors slowed the growth of V1-driven tumors but had little effect on V3 tumorigenesis, and vice versa.
Pharmacogenomic analyses revealed more. “We found that the drug response really depends on the fusion variant,” explained study author Mulham Najajreh, a PhD student at DKFZ. “Tumor cells carrying the V1 variant were much more sensitive to the ALK inhibitor lorlatinib, whereas those with the V3 variant showed resistance. Moreover, the loss of certain tumor suppressor genes—such as PTEN—further modified these drug responses, suggesting that a tumor’s complete genetic context influences treatment outcomes.
To confirm that these findings extend beyond mice, the researchers analyzed the largest available dataset of human EML4-ALK-positive lung cancers. They found that patients with different variants often carried different co-mutations, reinforcing the idea that these variants represent distinct biological entities.
“Our results show that not all EML4-ALK fusions are the same,” Sotillo said. “This could explain why some patients respond significantly better to therapies than others. In the long term, knowledge of the exact fusion variant could help to select treatments that are even more specifically tailored to the individual disease.”
By demonstrating that EML4-ALK variants differ in oncogenic potential, genetic dependencies, and drug sensitivity, the study challenges the long-standing practice of treating all ALK fusion–positive lung cancers identically. As precision oncology moves forward, the authors suggest that identifying a patient’s specific fusion variant—and accompanying tumor suppressor alterations—could become as critical as detecting the fusion itself.