When Muhammad Khatib, PhD, a Palestinian raised in Israel, now working at Stanford University as a postdoc, described his research to Inside Precision Medicine, there was a peaceful, restrained urgency behind his words. “I care a lot about human suffering,” Khatib said. “I want to use my expertise and skills to find ways to minimize it.”
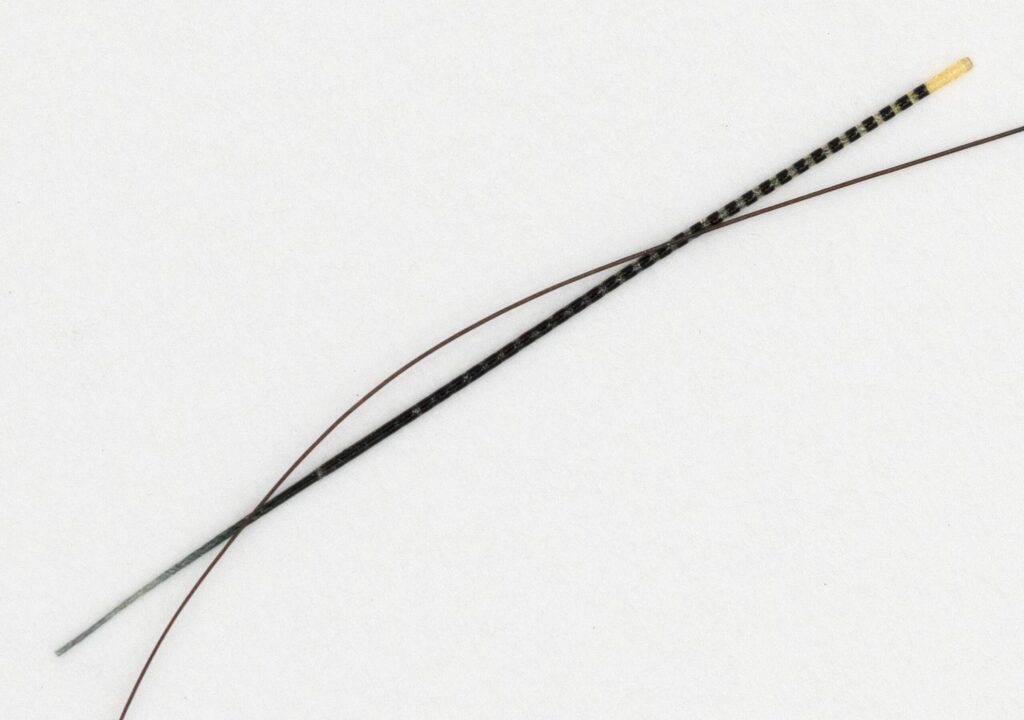
That mission has propelled Khatib from his hometown in Israel to Stanford University, where he is a postdoctoral researcher in the lab of chemical engineering professor Zhenan Bao, PhD. Their recent paper in Nature introduces NeuroString, a new class of electronic fibers thinner than a human hair and as soft as a rubber band. Implanted inside the body, these flexible devices can record, transmit, and even stimulate biological signals.

Although the new fibers carry “neuro” in their name, Khatib stresses that their potential isn’t limited to the nervous system. In early tests, they’ve monitored captured single-neuron activity in the brain and monitored gut function after surgery. “There will be many applications for NeuroString,” he said, “but we will also have other applications that are not related to neuro, such as pressure sensing and possibly impedance sensing, which have many applications and are relevant to many diseases.”
Khatib believes the possibilities—from smarter catheters to advanced brain-computer interfaces—are vast. In cardiology, for example, impedance sensing can reveal tissue properties or detect early signs of heart failure. In gastroenterology, pressure measurements could refine diagnostics for motility disorders. By enabling dense arrays of sensors in soft, stretchable formats, NeuroString could open entirely new diagnostic and therapeutic possibilities.
The mechanical mismatch problem
Khatib didn’t begin his scientific career imagining he’d work on devices destined for the human brain. As an undergraduate and then a doctoral student in chemical engineering at the Technion—Israel Institute of Technology, his interests centered on wearable electronics and synthetic skins that mimic human touch. But a pivotal realization changed his path.
“I found that working on medical devices could help treat some diseases or conditions in the future, combining my expertise and my personal passion,” he recalls. Implantable devices—electronics placed inside the body to sense or stimulate tissues—offered a direct way to improve patients’ lives.
Learning that Bao’s Stanford group was pushing the boundaries of soft, stretchable electronics inspired Khatib to cross continents. Bao, the K.K. Lee Professor of Chemical Engineering, is widely recognized for inventing flexible materials that behave like skin. Her lab had already demonstrated artificial skins that could “feel” pressure or temperature. NeuroString would extend that concept to the body itself.
Why is softness so important? Most medical implants are rigid. Neural probes, pacemaker leads, and intestinal sensors are typically made from stiff silicones or metals. But human tissues—especially the brain and gut—are squishy and constantly moving. When a stiff device presses against soft tissue, it can trigger an immune response, scar tissue formation, or even device failure.
“Our goal was to create devices and materials that were softer in order to reduce the severity of this mismatch,” Khatib explains. Rubber-like materials—technically, stretchable polymers—were the obvious choice. But integrating electronics into such materials at a microscopic scale is notoriously difficult. Traditional manufacturing methods are designed for flat, rigid wafers, not hair-thin, three-dimensional fibers.
The Bao lab’s breakthrough was to weave electronic sensors directly into ultra-thin, flexible fibers, allowing them to remain soft while carrying electrical signals. The result is a device with two key advantages. “The biggest advantage is the ability to integrate numerous devices, sensors, and electronic components onto a tiny fiber that is as thin as a human hair,” said Khatib. “The second advantage is that these fibers are made of rubber-like materials, making them very soft and stretchable.”

One of NeuroString’s most exciting demonstrations involved single-cell recordings in the brain. Capturing electrical activity from individual neurons is the gold standard for neuroscience research. While the brain garners much of the excitement, Khatib is equally enthusiastic about NeuroString’s gastrointestinal applications. After intestinal surgery, patients often experience temporary paralysis of the gut, called postoperative ileus, which can delay recovery and prolong hospital stays.
Currently, doctors have limited ways to monitor gut motility in real-time. NeuroString offers a potential solution: a flexible, implantable fiber that can track the gut’s electrical signals and even stimulate contractions when necessary. “We demonstrated that these devices can be utilized as non-invasive instruments to monitor adjustments in motility and, if necessary, stimulate the intestines during procedures to track recovery,” said Khatib.
Such monitoring could allow surgeons to detect problems earlier or tailor therapies for individual patients, improving outcomes and reducing healthcare costs.
From catheters to soft robots
NeuroString’s neuron recording capabilities are key for developing brain-computer interfaces (BCIs)—systems that translate brain activity into commands for computers or prosthetic limbs. “You may be familiar with Neuralink,” Khatib said, referencing Elon Musk’s high-profile BCI company. “We believe this technology will pave the way for new methods of brain interface and data recording, which will greatly advance the field.”
Because NeuroString can host far more electrodes in a much smaller footprint, it could allow neuroscientists to monitor larger populations of neurons without causing tissue damage. And its flexibility means it can move with the brain, maintaining contact without scarring.
Beyond BCIs, the fibers could improve deep brain stimulation (DBS), a therapy in which electrodes deliver controlled pulses to brain regions to treat Parkinson’s disease, epilepsy, or even depression. Today’s DBS systems are limited in how precisely they can target neurons. A dense, flexible array like NeuroString could enable more nuanced stimulation patterns—potentially improving symptoms or reducing side effects.
The team’s vision extends well beyond the brain and gut. Khatib said they’re exploring smart catheters and guide wires that could map pressures inside the heart or arteries, helping cardiologists treat arrhythmias or blocked vessels with greater precision. Flexible pressure sensors could also improve esophageal manometry—measuring how the esophagus contracts—to diagnose swallowing disorders.
“Without a doubt, those fibers have the potential to serve as the foundation for future wearable technology, electronic clothing, and soft robots,” Khatib adds. Devices that once had to remain outside the body—or be bulky and rigid—could one day be woven into fabrics or implanted unobtrusively.

NeuroString was not a solo achievement. “Conducting this type of research necessitates a wide range of expertise from various disciplines,” Khatib said. His own background is in electronic sensors and materials design, but the project required neuroscientists to test brain recordings, biologists to evaluate tissue compatibility, and electrical engineers to miniaturize circuits.
“If you look at the paper, you’ll notice that the authors come from almost every department, including every engineering department at Stanford,” he notes. “When we combine all of these skills, we can get to very exciting technologies and developments.”
This kind of collaboration mirrors broader trends in biomedical engineering, where solving complex problems—like making electronics work safely inside the body—requires teams that can cross traditional boundaries.
A personal turning point
While Khatib once envisioned a lifelong academic career, his perspective has shifted. “My lifelong goal of pursuing a career in academia began to shift in the last two years as I came to terms with the fact that, ultimately, helping alleviate human suffering was my true calling,” he said. “I have decided to leave academia and intend to do something more practical that will eventually benefit others.”
The plan? A startup to commercialize NeuroString and related technologies. But moving from the lab bench to the clinic is no small feat. The fibers will need to be manufactured at scale, integrated with control electronics, tested in animals and humans, and shepherded through regulatory approvals.
“Having the NeuroString alone isn’t enough to qualify it as a medical device,” Khatib explains. “It needs to be coupled with other components, such as electronic components for measurement, sensing, and stimulation… If that’s the case, NeuroString could work in a similar way [to a pacemaker]; the fibers would make direct touch with the body at the target area, and they’d be connected to an electrical component somewhere inside the body.”
Still, he’s optimistic. Collaborations with institutions like IMEC—the Belgian research center behind the widely used NeuroPixels probes—are already underway to develop human neural strings for recording brain signals. “Nearly every neuroscience lab around the globe uses [NeuroPixels],” Khatib notes. “We’ve been collaborating with them to develop human neural strings for recording brain signals, and I’m really excited about this direction.”
The transition from academic discovery to commercial product will require persistence. Manufacturing ultra-thin, sensor-packed fibers is tricky even under controlled lab conditions. Scaling production to meet regulatory standards for implants will take engineering ingenuity and capital. Long-term biocompatibility and durability must be proven in preclinical and clinical studies.
But Khatib is undeterred. “Being exposed to a lot of human suffering—even though I personally didn’t go through all of that—has changed the way I think about how to use my skills and expertise to make an impact in this world,” he said. “Helping alleviate human suffering is what will make me happy with what I do.”
If the technology delivers on its promise, future patients may recover faster after intestinal surgery, experience fewer complications from brain implants, or regain lost functions through sophisticated BCIs. Surgeons might one day rely on NeuroString-powered tools to navigate delicate procedures, while cardiologists map heart rhythms with unprecedented precision.
Soft, stretchable electronics could become as routine in medicine as today’s pacemakers or insulin pumps—thanks to a fiber thinner than a strand of hair and a researcher determined to turn science into relief.
A vision for science and society
For Khatib, the work is inseparable from his personal history. “I am Palestinian,” he said. “I grew up in Israel… We have a lot of similarities, and we hope for a better future.” He believes scientific collaboration can build bridges even when politics divides.
“Most people don’t want to combine what’s going on politically in the world with the world of science and technology, but I believe it’s very important to combine these two because the solution will come from people who care—who are passionate about making a positive impact in the world.”
By engaging with difficult conversations, Khatib hopes to show that shared values—compassion, curiosity, and the drive to help—can transcend borders. “It’s encouraging to see their growing interest,” he said of doctors and scientists eager to adopt NeuroString. “More feedback means we can believe in this technology even more.”