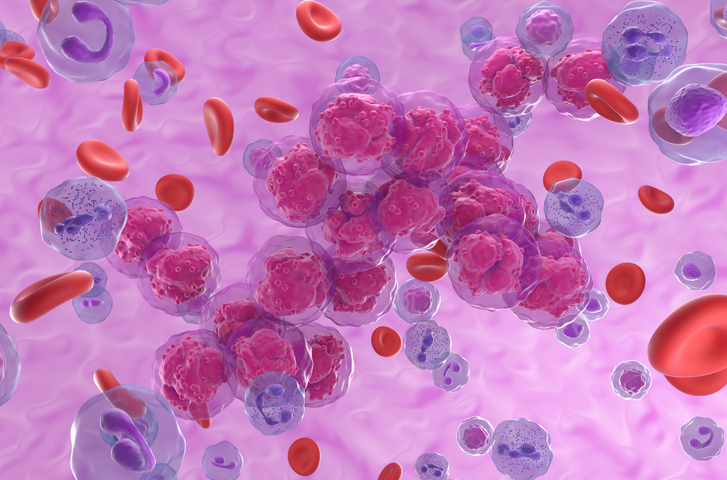
Cancer cells are metabolic opportunists, bending every pathway to fuel unchecked growth. Now UCLA scientists show that a single protein—Insulin-like Growth Factor 2 mRNA-Binding Protein 3 (IGF2BP3)—does double duty, rewiring leukemia metabolism and reshaping RNA regulation to keep malignant cells alive.
In a study titled “IGF2BP3 redirects glycolytic flux to promote one-carbon metabolism and RNA methylation,” published in Cell Reports Medicine, the researchers identify IGF2BP3 as a “master switch” that alters sugar breakdown and boosts leukemia proliferation by driving RNA modifications. Blocking this dual control, they suggest, could open new therapeutic avenues that starve cancer cells of both energy and survival signals.
IGF2BP3 belongs to a family of RNA-binding proteins that normally function only in early human development, helping guide mRNA localization, stability, and translation. After birth, these proteins are typically silenced—but in several cancers, including leukemia, they switch back on. Senior author Dinesh Rao, MD, PhD, professor of pathology and laboratory medicine at the David Geffen School of Medicine at UCLA, has tracked IGF2BP3 for nearly a decade. His group knew the protein was essential for aggressive pediatric acute lymphoblastic leukemia, but what remained unclear was how its oncogenic activity intersects with cellular metabolism.
To probe that question, the team turned to the Seahorse XF analysis, a technology that measures oxygen consumption and acid production, to reveal how these cells burn energy. Knocking out IGF2BP3 sharply reduced glycolysis, the quick but inefficient sugar-burning pathway favored by many cancers because it supplies building blocks for rapid growth.
“We expected IGF2BP3 might control RNA, but what we weren’t expecting was how strongly it also reshaped metabolism,” Rao said. “That connection hadn’t been seen before and could be critical to how cancer cells gain their advantage. By uncovering this link, we now have a clearer picture of how leukemia sustains itself. If we can block this rewiring, we might be able to cut off both the energy supply and the survival signals cancer cells rely on.”
Further metabolic profiling revealed a chain reaction. Without IGF2BP3, levels of S-adenosyl methionine (SAM)—the key methyl-group donor for RNA modification fell dramatically. The team wrote that using enhanced Crosslinking Immunoprecipitation (eCLIP) and polyribosome profiling, they found that IGF2BP3 promotes translation of the regulatory subunit of the methionine adenosyltransferase complex (MAT2B), involved in SAM production.
“When we removed IGF2BP3, it didn’t just change how cells used energy,” noted postdoctoral scholar Gunjan Sharma, PhD. “It also disrupted their chemical balance and the way their RNA was regulated. That’s how we realized IGF2BP3 links metabolism and RNA control in leukemia.”
The researchers wrote, “…these data suggest the intriguing hypothesis that IGF2BP3 rewrites the epitranscriptome in leukemia cells.” The discovery positions IGF2BP3 as a potential therapeutic target and biomarker. Rao’s group is now testing small molecules that inhibit the protein, with the most promising strategies pairing such inhibitors with drugs that interfere with cancer metabolism. They continued, “This work highlights an interconnection between oncogenic metabolism and RNA modifications, suggesting that pervasive gene expression changes necessary for oncogenesis may be perpetuated by post-transcriptional gene regulation.”
Although the current work centers on leukemia, the researchers believe similar metabolic–RNA circuits may fuel other malignancies, broadening the clinical impact of this “master planner” protein.