An mRNA vaccine suppressed neovascularization—a condition caused by age-related macular degeneration (AMD), a leading cause of vision loss for elderly people—in the retina of mouse models. The vaccine can be delivered intramuscularly and offers a more comfortable and easier-to-administer alternative for treating AMD and other neovascular eye diseases.
This research is published in Vaccine in the paper, “mRNA vaccination mitigates pathological retinochoroidal neovascularization in animal models.”
AMD is one of the leading causes of vision loss in people over 60 years; the condition affects nearly 200 million people worldwide. One form of the disease, known as wet AMD, is caused by neovascularization (the growth of abnormal vessels in the eye). These blood vessels leak fluid buildup in the retina, which gradually leads to vision loss if left untreated. At present, the only way to slow this process is through regular injections of anti-angiogenic drugs that stop the formation of blood vessels directly into the eye. However, these must be taken regularly, and patients can stop responding to the treatment.
Now, researchers at Institute of Science Tokyo, Japan, have developed a novel mRNA vaccine that can be injected intramuscularly, making it easier to administer and less burdensome on patients than current treatments that require direct injections into the eye. The vaccine was tested in mice and shown to strongly suppress retinochoroidal neovascularization.
“The COVID-19 pandemic highlighted the remarkable potential of mRNA as a vaccine platform. Inspired by those successes, we sought to expand its use beyond infectious diseases and cancer to chronic eye conditions. To our knowledge, this is the first study to show that an mRNA vaccine can suppress pathological neovascularization in animal models,” says Satoshi Uchida, MD, PhD, professor of the Department of Advanced Nanomedical Engineering, Institute of Science Tokyo.
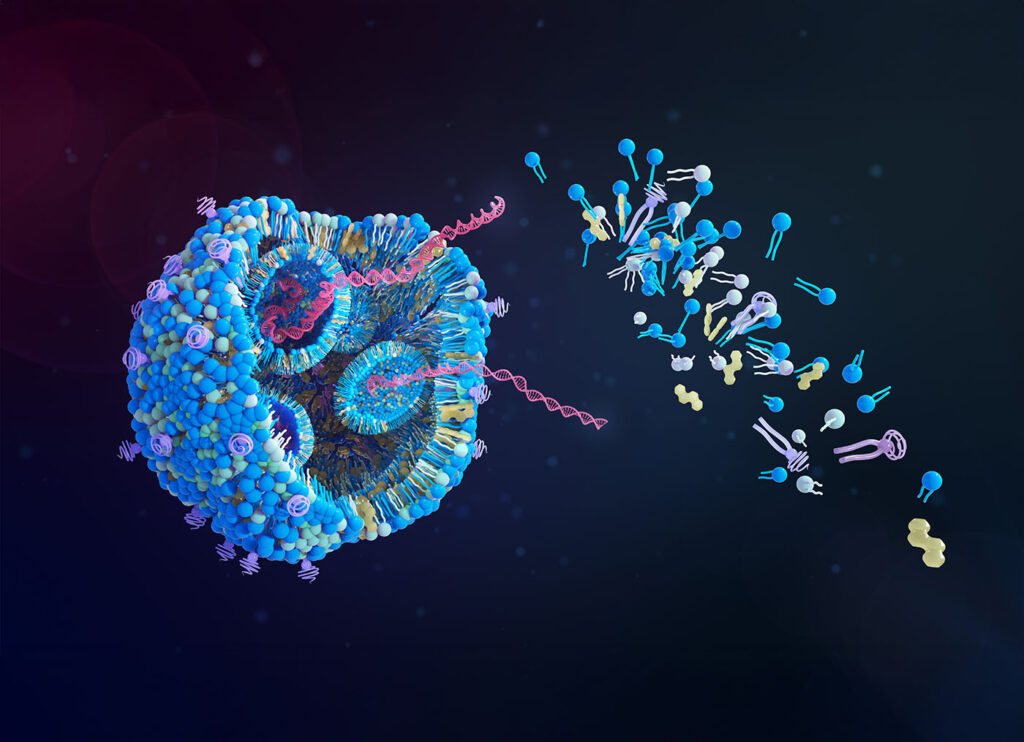
The vaccine delivers mRNA encoding leucine-rich alpha-2-glycoprotein 1 (LRG1), a protein known to promote angiogenesis and found in elevated levels in patients with AMD. As a result, the body produces antibodies that specifically bind to and inhibit LRG1.
The researchers tested the vaccine on two mouse models of eye disease: one in which choroidal neovascularization (CNV) was induced, and another that naturally develops CNV. After just two intramuscular injections given 14 days apart, both models showed strong antibody responses that significantly reduced abnormal blood vessel growth in the retina. The effects were visible within a week of the first dose. By the 21st day, the laser-induced CNV model showed an 85% reduction in leakage and an 82% reduction in lesion size. In the natural NV model, lesion size decreased by 55% on the 28th day.
More specifically, the authors write: “In a laser-induced NV model, the LRG1 mRNA vaccine reduces NV area and leakage while inhibiting microglial cell infiltration. Histological analysis shows no adverse effects on retinal architecture or glial cell activation. Additionally, in Vldlr knockout mice, LRG1 mRNA administration suppresses ongoing neovascularization and downregulates key angiogenic mediators.”
Also, the vaccine appeared safe: it did not interfere with normal blood vessel growth, damage healthy retinal tissue, or trigger harmful immune reactions in other organs of the mice. At the same time, the treatment was as effective as standard anti-vascular endothelial growth factor (VEGF) drugs, yet free from their major drawbacks.
“The effects of LRG1 mRNA vaccination on reducing endothelial and microglial cells were comparable to those of anti-VEGF antibody therapy,” says Uchida. “Unlike conventional treatments requiring repeated intravitreal injections, this vaccine may provide long-term benefits with a single intramuscular dose, potentially reducing the treatment burden for patients.”