A new approach to CAR T cell therapy, involving engineering the cells to produce fusion proteins combining a cytokine and an antibody, has shown improved efficacy and safety in animal models of prostate and ovarian cancer. Published in Nature Biomedical Engineering, results of the study show early promise to enhance the performance of this therapeutic modality in solid tumors, which make up about 90% of cancer diagnoses.
“We believe this new strategy will provide a productive boost to current CAR T cell therapies and can be applicable to multiple cancer types,” said John P. Murad, PhD, assistant professor of research in the department of medicine at the Keck School of Medicine of the University of Southern California and lead author of the study.
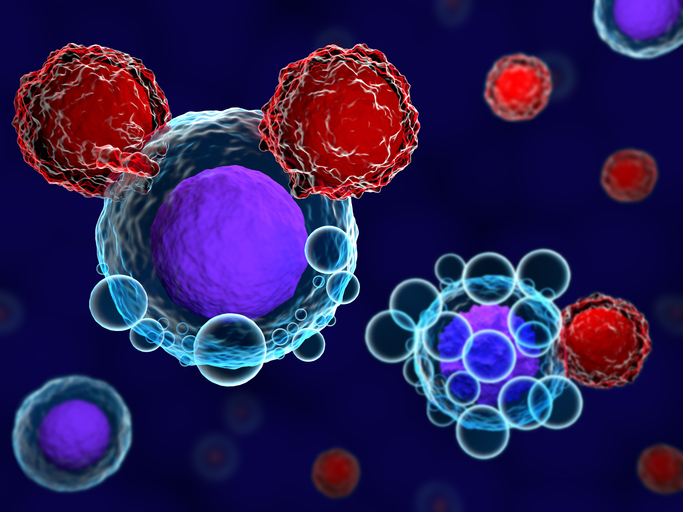
Historically, CAR T therapy has failed to be as effective in solid tumors as it is in liquid cancers such as lymphoma or leukemia. A major reason for this limitation is the immunosuppressive tumor microenvironment often found in solid tumors, which dampens the T cell response and limits tumor infiltration.
Previous studies had looked into combining CAR T cells with cytokines in order to enhance the immune response. However, administering cytokines systemically can cause toxicity across the body and potentially trigger cytokine release syndrome, a common side effect of CAR T therapy that can be deadly in the most severe cases.
The new approach designed by Murad and colleagues works around these limitations by delivering cytokines only in the area where the tumor is located. This was achieved by engineering the CAR T cells to produce fusion proteins combining an antibody targeting the programmed death-ligand 1 (PD-L1) with interleukin 12 (IL-12) into a single molecule. As the tumor raises PD-L1 levels, the anti-PD-L1 antibody naturally gathers in and around the tumor, allowing IL-12 to act locally.
“By designing CAR T cells that release both IL-12 and a PD-L1 blocker as a fusion protein, we can make the treatment safe and also much more effective, even against tumors that usually resist CAR T cell therapy,” said senior author Saul Priceman, PhD, associate professor in the department of medicine at the Keck School of Medicine and founding director of the Norris Center for Cancer Cellular Immunotherapy Research.
These CAR T cells were tested in human cells and in mouse models of ovarian and prostate cancer, where the approach proved highly effective at shrinking the tumors. Overall, the treatment showed minimal systemic toxicity while enhancing the ability of T cells to penetrate the tumor and modifying the tumor microenvironment to make it less hostile to immune cells.
While more research will be needed to confirm these initial findings, the researchers are confident that this approach could be applied to a wide range of solid tumors. Studies are already underway testing these engineered CAR T cells in pancreatic cancer, soon to be followed by colorectal cancer and brain tumors. Furthermore, a similar strategy could be used to improve the efficacy of immunotherapies involving other immune cells, such as NK cells or macrophages. Clinical trials are expected to start within the next one to two years.
“No two cancers are the same, so each needs to be tested and validated as a potential clinical approach,” said Priceman. “But the new therapy could have broad applicability, because most solid tumors create a surrounding environment that weakens the immune system, which we are capitalizing on with this strategy.”