Depression is a debilitating mental health disorder that remains a substantial global health challenge. Despite the availability of various antidepressants, treatment outcomes often face limited efficacy, delayed onset of action, and adverse effects. These drugs focus on regulating neurotransmitters, especially serotonin, and benefit only about half of patients. This limitation emphasizes the need to search for new molecular pathways in the brain beyond neurotransmitter signaling to treat mental health disorders.
In a new study published in Science Advances titled, “Abnormal O-glycan sialylation in the mPFC contributes to depressive-like behaviors in male mice,” researchers from the Institute for Basic Science (IBS) have identified a new molecular pathway in the mouse brain that directly links abnormal sugar modifications on proteins to depressive behaviors. Notably, chronic stress disrupts O-glycans attached to proteins in the prefrontal cortex to trigger depression. The findings open new possibilities for targeted therapies for treatment-resistant depression.
Post-translational modifications (PTMs) have recently emerged as a promising frontier in understanding brain disorders, offering insights into molecular mechanisms beyond genes and proteins. Glycosylation, a biochemical process involving the attachment of sugars to proteins or lipids, is one of the most complex PTMs. Despite its critical role in protein function, stability, and key biological processes such as glucose metabolism, cell signaling, and immune responses, the functional implications of glycosylation remains underexplored.
“This study demonstrates that abnormal glycosylation in the brain is directly connected to the onset of depression,” said Boyoung Lee, PhD, principal investigator at the Center for Cognition and Sociality at IBS and corresponding author of the study. “It provides an important foothold for identifying new diagnostic markers and therapeutic targets beyond neurotransmitters.”
Using high-performance mass spectrometry, the team identified distinct glycosylation features in nine brain regions of healthy mice. When compared to the brains of chronically stressed mice, results showed significant alternations in O-glycosylation in regions, such as the prefrontal cortex, including a reduction in sialylation and decreased expression of the enzyme St3gal1, which mediates this modification.
Suppressing St3gal1 in healthy mice caused depressive-like symptoms, including loss of motivation and heightened anxiety even without stress. Conversely, increasing St3gal1 in stressed mice alleviated their depressive behaviors. These results support decreased St3gal1 as a key molecular factor that directly induces and regulates depressive symptoms.
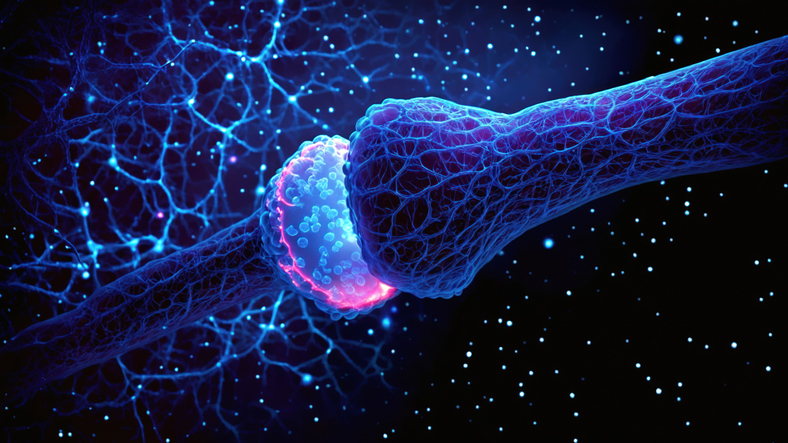
Further protein analyses and electrophysiological experiments showed that reduced St3gal1 destabilized the sugar chain structures of synaptic molecules, including neurexin 2 (NRXN2), a synaptic adhesion protein, and impaired the function of inhibitory neurons that normally help maintain balance in brain circuits. These findings suggest that small changes in sugar chains simultaneously disrupted both the connections and stability of neural circuits to impact the brain’s emotion-regulation system.
“Depression imposes a major social burden, yet current treatments remain limited,” said C. Justin Lee, PhD, co-director of the Center for Cognition and Sociality at IBS and co-author of the study. “This achievement could extend not only to depression therapy but also to other mental illnesses such as PTSD and schizophrenia, paving the way for broader therapeutic strategies.”