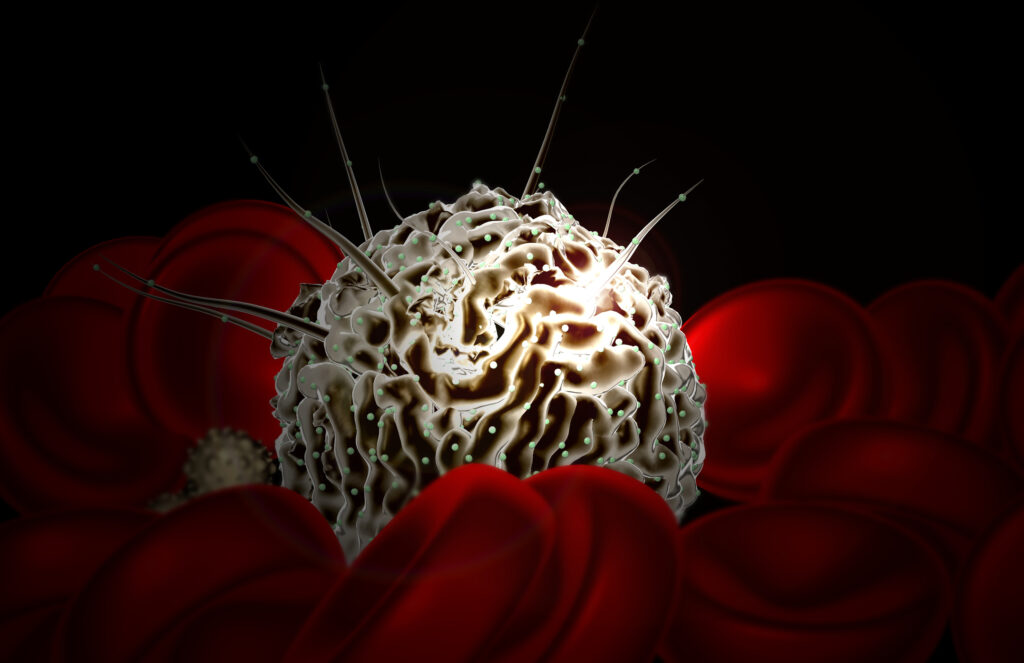
Researchers at the University of Cambridge have developed embryo-like structures that mimic aspects of early human development, including the production of blood stem cells. These new self-organizing embryo-like structures were developed using human pluripotent stem cells (hPSCs) to produce three-dimensional structures, dubbed “hematoids,” which simulate post-gastrulation human embryogenesis and, within about two weeks, begin producing hematopoietic stem cells (HSCs) that can differentiate into both red and white blood cells.
“It was an exciting moment when the blood red color appeared in the dish—it was visible even to the naked eye,” said Jitesh Neupane, PhD, a stem cell and developmental biologist at the University of Cambridge’s Gurdon Institute and first author of the study, published in Cell Reports.
The researchers noted that the hematoids also contain beating heart cells and liver-like cells, recapitulating features of human embryos at Carnegie stage 12–16, and provide the basis for a fertile avenue of researching blood diseases such as leukemia. There is also the potential to develop a platform for producing long-lasting blood stem cells for transplant.
Unlike other lab-based methods of producing blood stem cells, this new approach does not rely on the addition of external proteins, growth factors, or forced gene expression, rather the hematoids form through a self-directed developmental process using a single small-molecule inhibitor of TGF-β1 to guide their growth. “There is no requirement for exogenous supplementation with hematopoiesis-associated cytokines, growth factors, or ectopic transcription factor over-expression,” the researchers wrote. “Hematoids provide a versatile model of the endogenous human hemogenic niche, setting this system apart from traditional EB-based approaches.”
Once they were developed, the investigators then explored how hematoid-derived blood stem cells function. Using a co-culture system, they demonstrated that these cells can give rise to multiple blood lineages, including T cells and natural killer cells. “The maturation of CD3+ T cells and CD3−CD56+ NK cells from hematoid-derived HSCs strongly suggests that these cells are not myeloid-restricted primitive HSCs derived from the yolk sac,” the researchers wrote.
The hope is that hematoids could help provide a deeper, more detailed understanding of blood diseases that arise early in life, such as leukemia, by allowing researchers to simulate disease development in a controlled laboratory setting.
“Hematoids capture the second wave of blood development that can give rise to specialized immune cells or adaptive lymphoid cells, like T cells opening up exciting avenues for their use in modeling healthy and cancerous blood development,” said co-first author Geraldine Jowett, PhD, a researcher at University of Cambridge’s Gurdon Institute.
The investigators noted there is great promise for hematoids to make a significant impact in precision medicine. Since the human stems cells that are used to create hematoids could be derived from a patient’s own cells, it could be possible to create blood stem cells that are immunologically compatible with the patients.
Senior author Azim Surani, PhD, director of germline and epigenetics research at the Gurdon Institute said, “This model offers a powerful new way to study blood development in the early human embryo. Although it is still in the early stages, the ability to produce human blood cells in the lab marks a significant step towards future regenerative therapies—which use a patient’s own cells to repair and regenerate damaged tissues.”
The Cambridge researchers are now working to refine the hematoid model to improve the maturation and functional output of the hematopoietic stem cells and are exploring the generation of additional immune and blood cell subtypes.