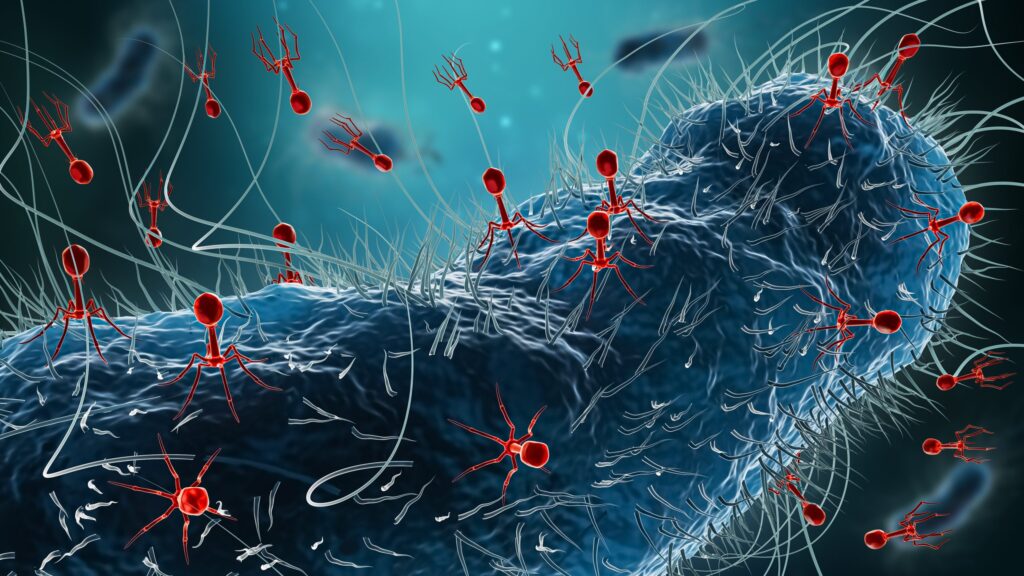
Although it well known that the human gut contains a large and diverse array of bacteriophages, a functional understanding of the phage–host interactions is limited. This is, in part, due to a lack of cultured isolates available. Now, a new study uncovers hundreds of new phages within our gut, information that could eventually reshape the gut microbiome, potentially influencing gut health and the progression of various disease states.
Published in Nature in the paper, “Isolation, engineering and ecology of temperate phages from the human gut,” the study is the first of its kind and uses a large-scale, culture-based approach to isolate and study temperate bacteriophages in the human gut.
“This is a foundational study that changes how we think about and study the viruses within the human gut,” said Jeremy Barr, PhD, professor at the Monash University’s School of Biological Sciences. “We found that compounds produced in human gut cells can wake up dormant viruses inside gut bacteria. This could have major implications for gut diseases like inflammatory bowel disease (IBD), where inflammation and cell death are common.”
The research team worked with 252 bacterial isolates from the human microbiome, which were sourced from the Australian Microbiome Culture Collection (AusMiCC). The isolates were grown using anaerobic chambers and then treated with ten diverse compounds, foods, and conditions.
More specifically, the researchers characterized 134 inducible prophages from the 252 isolates using 10 different induction conditions to expand the experimentally validated temperate phage–host pairs originating from the human gut. Importantly, they write, only 18% of computationally predicted prophages could be induced in pure cultures.
The study revealed that most gut bacteriophages are dormant, with only a small fraction capable of being activated under the tested conditions. However, when exposed to human gut cells, the activation rate of these viruses jumped significantly. More specifically, the team constructed a 78-member synthetic microbiome that, when co-cultured in the presence of human colonic cells (Caco2), led to the induction of 35% phage species. This suggests that human biology plays an important and direct role in shaping the viral landscape of the gut. Interestingly, the team found that Stevia, a common plant-based sugar substitute, and compounds released by our own gut cells, were leading activators for gut phages.
“We’ve known that the gut is full of viruses, but until now, we didn’t have the tools and experimental approaches to study them in the lab,” explained Sofia Dahlman, a graduate student in the Barr lab. “Our findings suggest that the human host isn’t just a passive environment, it’s actively influencing viral behavior.”
Using CRISPR-based genetic engineering, the team further identified mutations in viral genes that prevent activation, offering insight into how some gut viruses become permanently dormant. This discovery could inform future therapeutic strategies aimed at manipulating the gut microbiome for health benefits.
“Being able to grow these viruses allows us to understand their function and provides the opportunity to develop microbiome therapeutics for diseases from inflammatory bowel disease to cancers,” notes Forster. “This technology also provides a capacity to engineer probiotic strains with tailored viral functions,” he said.