Faulty brain circuits seen in Down syndrome may be caused by the lack of a particular molecule essential for the development and function of the nervous system, according to a new study in lab mice. Restoring the molecule, called pleiotrophin, could improve brain function in Down syndrome and other neurological diseases, possibly even in adults, the researchers say.
The scientists conducted their work in mice, rather than in people, so the approach is far from being available as a treatment. But the researchers found that administering pleiotrophin improved brain function in adult mice long after the brain was fully formed. That suggests that the approach could offer major advantages over prior attempts to enhance Down syndrome brain circuits that would have required intervention at extremely precise, and brief, times during pregnancy.
“This study is exciting because it serves as proof-of-concept that we can target astrocytes, a cell type in the brain specialized for secreting synapse-modulating molecules, to rewire the brain circuity at adult ages,” said researcher Ashley N. Brandebura, PhD, who was part of the research team while at the Salk Institute for Biological Studies and is now part of the University of Virginia School of Medicine. “This is still far off from use in humans, but it gives us hope that secreted molecules can be delivered with effective gene therapies or potentially protein infusions to improve quality of life in Down syndrome.”
Understanding Down syndrome
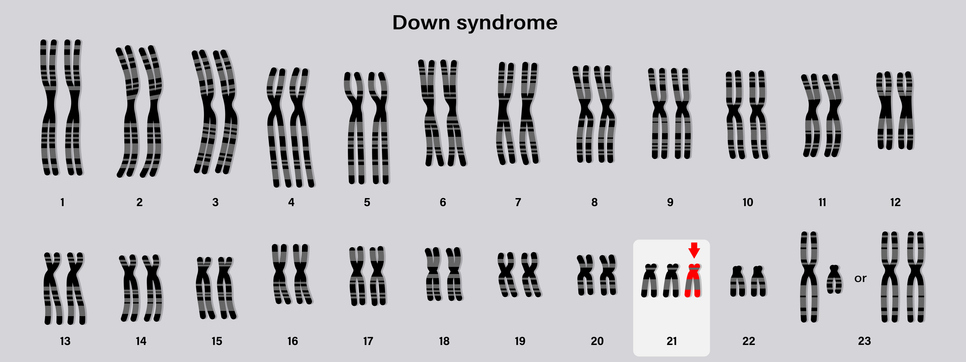
Down syndrome affects approximately one in 640 babies born each year in the U.S., according to the federal Centers for Disease Control and Prevention. Caused by a mistake in cell division during development, the condition can lead to developmental delays, hyperactivity, shortened lifespan, and increased risk for medical problems such as heart defects, thyroid issues, and problems with hearing and vision.
Salk researchers, led by Nicola J. Allen, PhD, wanted to better understand the causes of Down syndrome, so they looked for cellular proteins altered in the brains of lab mice used to model the condition. The scientists identified pleiotrophin as a promising candidate because it is present at high levels at critical moments in brain development and because it plays essential roles in the formation of brain synapses and in the development of axons and dendrites. Further, the presence of the protein is reduced in Down syndrome. To determine if restoring pleiotrophin would improve brain function, the researchers delivered it where it was needed using viral vectors.
The researchers found that administering pleiotrophin to astrocytes had big benefits, including increasing the number of synapses in the hippocampus region of the brain. Further, it increased brain plasticity (the ability to form or modify connections essential for learning and memory).
“These results suggest we can use astrocytes as vectors to deliver plasticity-inducing molecules to the brain,” Allen said. “This could one day allow us to rewire faulty connections and improve brain performance.”
While the findings are promising, the scientists don’t believe that pleiotrophin is the only cause of brain circuit problems in Down syndrome. Further research is needed to understand the complex contributors to the condition, they caution. But their work, they say, provides proof of the viability of an approach that could be beneficial not just for Down syndrome, but other neurological diseases as well.
“This idea that astrocytes can deliver molecules to induce brain plasticity has implications for many neurological disorders, including other neurodevelopmental disorders like fragile X syndrome but also maybe even to neurodegenerative disorders like Alzheimer’s disease,” Brandebura said. “If we can figure out how to ‘reprogram’ disordered astrocytes to deliver synaptogenic molecules, we can have some greatly beneficial impact on many different disease states.”
Having completed her postdoctoral studies at Salk, Brandebura plans to continue her research in her new post at UVA Health, where she is a member of the UVA Brain Institute, the department of neuroscience and the Center for Brain Immunology and Science and the Center for Brain Immunology and Glia.