A polarized debate in biomedical research is pitting those who favour ‘traditional animal models’ — meaning living non-human mammals, such as mice, that are used to investigate human disease mechanisms, responses to treatments and so on — against proponents of various experimental approaches collectively termed NAMs.
NAMs, short for ‘new approach methodologies’ or ‘novel alternative methods’, include in vitro models, such as organoids grown from stem cells or other cells, that are designed to mimic the properties of human organs or tissues1; computational (in silico) modelling approaches that predict how biological systems respond to drugs or other perturbations2; and chemical (in chemico) techniques that assess how biological molecules interact outside an organism or cell3.
NAMs could markedly accelerate progress in drug discovery, toxicology and disease modelling. They could also lessen the need for animal testing, which is ethically problematic for many people. But framing NAMs as innovative disrupters and ‘traditional animal models’ as outdated holdovers — as many are now doing — oversimplifies a reality that is much more nuanced. Worse, it is distracting researchers from considering the scientific, ethical and translational issues related to both types of approach.
Complementary approaches
As a clinically trained veterinarian and biomedical scientist, I have been using mouse models to try to understand human genetic diseases for more than 20 years. The principles driving the development of NAMs are not new. For decades, researchers have been using tools, such as human induced pluripotent stem cells, to garner information relevant to humans and to lessen the need for animal testing. What’s brought all this to the fore are major technological advances in NAMs and a push by regulators and funders globally for the expanded use of these methods in research.
But instead of asking whether ‘to NAM or not to NAM?’ when considering the use of anything as a research model, the question should be: ‘Does the model I am using faithfully represent the biological system I am studying?’
Alternatives to animal testing are the future — it’s time that journals, funders and scientists embrace them
NAMs and animal models offer distinct, often complementary insights into the workings of complex in vivo biological systems. For well-defined, narrow applications, such as in toxicology, or when researchers are wanting to assess a specific biological process or disease mechanism at the molecular, chemical, cellular or organ level, NAMs are proving highly useful. Currently, however, no NAM can model how a specific gene functions in a person, how an organ or the entire body works or how a disease progresses.
All models — whether they are NAMs or inbred mice — should be updated, refined or replaced as tools and data emerge that allow researchers to better match models to the human system they are trying to investigate.
Experimental technologies, such as the gene-editing tool4 CRISPR–Cas9, have made it easier for researchers to design animal models that more faithfully recapitulate human biological processes or phenomena. Targeted genome editing in mice5, for instance, has shown how some human genes have different effects in men and women6, and how some have different effects at different life stages7. It has also uncovered cases of genetic pleiotropy, in which a single gene influences multiple traits8,9. Future advances will probably improve animal models even further.
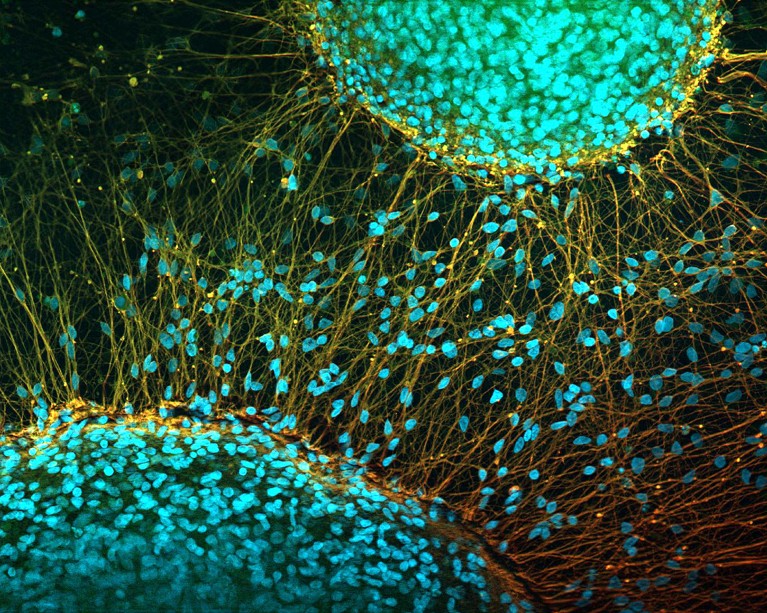
Nerve cells derived from human induced pluripotent stem cells.Credit: Ikelos/Dr Christopher B. Jackson/SPL
Moreover, for all models, the quality and usefulness of the information generated will depend on a host of factors that are extraneous to the model itself.
NAMs are increasingly being touted as a solution for the limited translatability of findings from preclinical research to the clinic10. On average, 86% of drug candidates fail in clinical trials10, and some of these failures have been linked to the use of animal models11.
But problems with translatability can stem from factors other than the physiological differences between species12,13. For instance, the disease models could have been oversimplified, or the group sizes made too small, or the animals being tested might not have been assigned to the treatment groups in a sufficiently random manner. Many of these issues could apply equally to studies involving NAMs.

