The ovary ages decades ahead of other organs in the body. Vitamin C slowed that aging process in middle-aged macaques.
The ovary ages long before the rest of the body. By the time people enter their thirties, egg supply dwindles, hormones fluctuate, and fertility falls. Scientists have long wondered why this small organ wears out decades ahead of others, and whether its clock can ever be slowed.1 Unlike the brain or the heart, the ovary’s regenerative capacity seems fixed, yet recent work in non-human primates hints that this assumption may not hold.
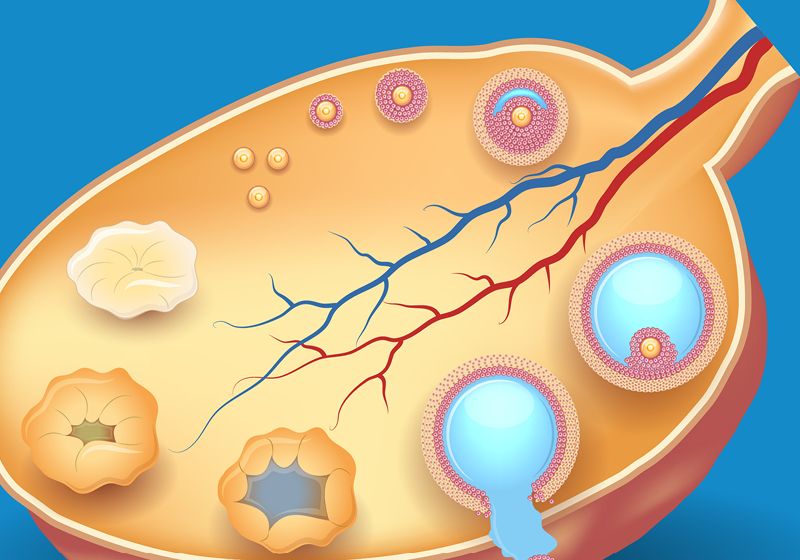
In a long-term study published in Cell Stem Cell, Guang-Hui Liu, a regenerative medicine researcher at the Chinese Academy of Sciences, and his colleagues reported that middle-aged macaques receiving a moderate daily dose of vitamin C showed healthier follicles and improved ovarian vasculature, suggesting reduced cellular stress.2 The findings suggest that the simple nutrient might slow molecular aging in one of the body’s most time-sensitive organs.
To investigate how vitamin C influenced cellular aging, Liu’s team analyzed ovarian tissue from treated and untreated macaques after 3.3 years of supplementation—roughly equivalent to a decade of human aging. The animals had received about 30 milligrams of vitamin C per kilogram of body weight each day during this period. The researchers then mapped the genetic signatures of thousands of macaque ovarian and somatic cells using single-cell transcriptomics.
The researchers found that vitamin C treatment reactivated antioxidant defenses through Nuclear factor erythroid 2-related factor 2 (NRF2), a transcription factor whose expression and activity wanes in aged macaques.3 “NRF2 was a key mediator of vitamin C’s benefits, particularly in reducing oxidative stress and inflammation,” said Liu. This restoration boosted antioxidant enzymes such as glutathione peroxidase 1 and NAD(P)H:quinone oxidoreductase 1 (NQO1), while dampening pro-inflammatory and senescence-related genes. The treatment also recalibrated iron metabolism—reducing the buildup of iron ions that can damage cell membranes—and enhanced mitochondrial maintenance and energy production. These molecular effects were reflected at the tissue level as well. Mitochondria appeared structurally healthier, fibrosis had declined, and endothelial cells that sustain the ovary’s blood vessels showed stronger integrity and less inflammation.
When the team used these data to build a single-cell “aging clock”—a computational model that estimates a cell’s biological age from its gene-expression profile—they found that oocytes appeared about 1.35 years younger, and the surrounding somatic cells looked younger by 5.66 years compared with untreated animals. Similar gene expression patterns emerged when the researchers exposed human ovarian cells to vitamin C in culture, hinting that the mechanism may extend beyond macaques and into human biology.
However, translating these cellular gains into fertility remains uncharted. Cellular youth does not necessarily mean reproductive youth. The researchers didn’t track pregnancy rates, live births, or egg quality, and while they found that vitamin C preserved anti-Müllerian hormone (AMH) expression in ovarian tissue—a local indicator of follicular function—they didn’t measure circulating AMH or other fertility outcomes. “[These markers] are what we care about in the fertility world,” said Zaher Merhi, the medical director of Rejuvenating Fertility Center, who was not associated with the new study.
Other experts described the findings as both an advance and an invitation to dig deeper. “This study takes a large step forward in demonstrating that a single antioxidant compound can have geroprotective effects in a nonhuman primate,” said reproductive biologist Francesca Elizabeth Duncan of Northwestern University, who was not associated with the study. She noted that vitamin C’s established safety and the fact that humans and macaques metabolize it similarly make it an attractive candidate for translation. Going forward, she said researchers need to learn whether vitamin C acts directly on the ovary or systemically, and how the timing and dose of its administration affect long-term outcomes.
Evelyn Telfer, a reproductive biologist at the University of Edinburgh, who was not associated with the study, noted that oxidative damage contributes to aging not only in ovaries but also in the brain, heart, and kidneys—raising the possibility that similar interventions might benefit other organs. She cautioned that “antioxidant effects are dose dependent, and high doses can be damaging, particularly to cell-repair capacity.” Human data, she added, remain limited. Antioxidant trials such as those testing vitamin C and E, coenzyme Q10, and β-carotene in aging-associated diseases such as diabetes and cardiovascular disorders have so far yielded mixed results.4 In her own work growing human ovarian tissue in vitro, she finds that antioxidant form and concentration can either support or impair follicle growth and somatic cell health, depending on the balance.
For Liu, that test is already underway. “As a next step, our team plans to launch a clinical trial that uses a human composite aging clock as one of the primary endpoints to test whether vitamin C can slow human aging—including reproductive aging,” he said. It remains to be seen if vitamin C can slow reproductive aging in humans, but the primate data suggest that even the ovary’s clock may not be immutable.