Type 1 diabetes is an autoimmune disease in which the body destroys its own insulin-producing beta-cells in the pancreas, leaving patients with a lifelong dependency on external insulin. Children whose parents or siblings have type 1 diabetes possess an eight to 15-fold increased risk of developing the autoimmune disease. Research suggests that early-life epigenetic programming may be a key mechanism through which maternal type 1 diabetes confers a protective effect.
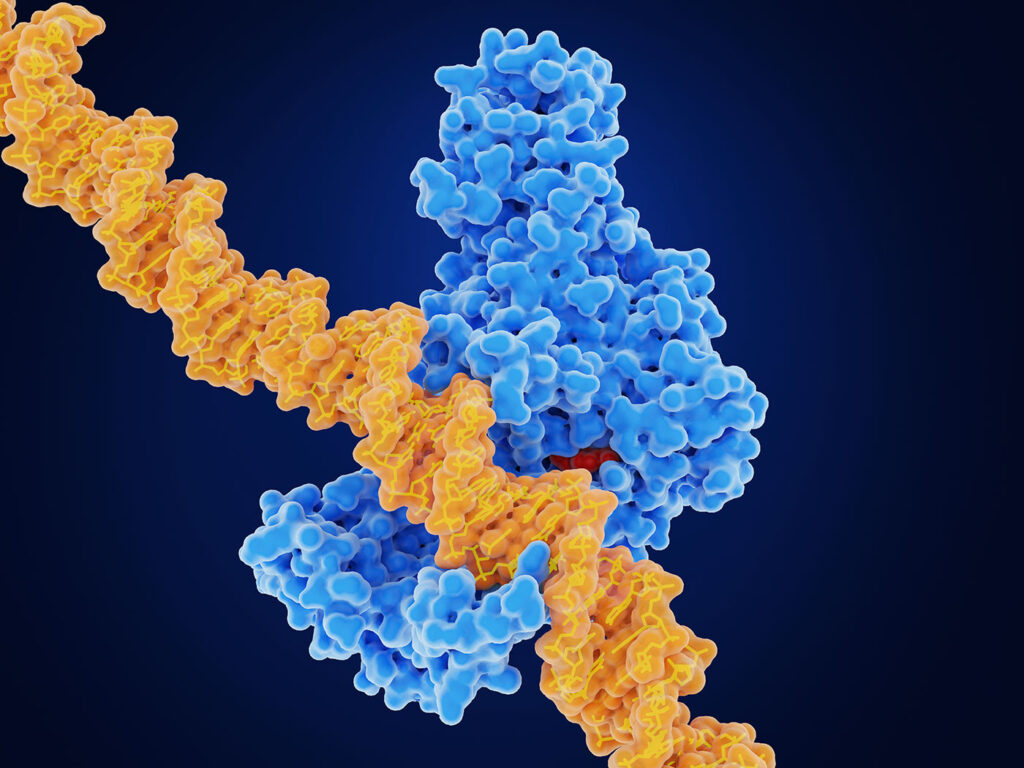
In a new study published in Nature Metabolism titled, “Blood methylome signatures in children exposed to maternal type 1 diabetes are linked to protection against islet autoimmunity,” researchers from Helmholtz Munich demonstrate that maternal type 1 diabetes is associated with specific epigenetic marks in the form of DNA methylation in the child. These changes appear to affect the expression of several genes involved in immune function.
“We observed DNA methylation changes at multiple type 1 diabetes susceptibility genes in children born to mothers with type 1 diabetes,” said Sandra Hummel, PhD, professor at the Helmholtz Munich Institute for Diabetes Research and corresponding author of the study.
Environmental influences in the womb such as smoking by the mother, medical conditions, stress, or diet can have far-reaching effects on a child’s health by changing DNA methylation patterns. The intrauterine environment may influence the child’s risk for islet autoimmunity through epigenetic modifications.
The authors examined blood samples from 1,752 children at around two years of age from the BABYDIAB, BABYDIET, and POInT cohorts. All children included had an increased genetic risk for type 1 diabetes. They compared DNA methylation patterns of 790 children with and 962 children without a mother affected by type 1 diabetes to identify differences linked to maternal diabetes.
“Our study identified numerous differentially methylated genetic locations, predominantly in the HOXA gene cluster and the MHC region in offspring of mothers with type 1 diabetes. The MHC region is known to confer the major genetic susceptibility and resistance to type 1 diabetes,” said Raffael Ott, PhD, lead scientist at the Institute of Diabetes Research and first author of the study. “We observed that the epigenomic changes in these children were associated with the expression of 15 type 1 diabetes susceptibility genes.”
Using 34 differentially methylated positions at type 1 diabetes susceptibility loci that best reflected exposure to maternal type 1 diabetes, the researchers created a methylation propensity score. Results showed that children without a mother with type 1 diabetes developed islet autoimmunity and had significantly lower scores, indicating less protective epigenetic modification.
In a follow-up project, Hummel along with Ezio Bonifacio, PhD, group leader at the Center for Regenerative Therapies Dresden at the TU Dresden University of Technology, will aim to identify which type 1 diabetes susceptibility genes are epigenetically modulated by maternal type 1 diabetes. Researchers will also investigate whether similar epigenetic effects occur in children born to mothers with gestational diabetes.
In collaboration with Helmholtz Munich, the project will also explore potential protein and metabolomic biomarkers linked to DNA methylation patterns and how these molecular changes contribute to protection against islet autoimmunity.