Serious damage to short-term kidney function, known as acute kidney injury (AKI) can be fatal and also increase the risk of irreversible chronic kidney disease. It may be triggered by stressors ranging from sepsis to heart surgery, and affects more than half of ICU patients.
Researchers at University of Utah Health (U of U Health) have now reported the results of preclinical in vitro experiments and studies in live mice suggesting that AKI is triggered by fatty molecules called ceramides, which cause serious injury by damaging kidney mitochondria in proximal tubules (PTs).
The team found that tweaking how ceramides are made, either genetically or using a drug, kept mitochondria healthy and functional even under stress. “We completely reversed the pathology of acute kidney injury by inactivating ceramides,” said Scott Summers, PhD, distinguished professor and chair of the Department of Nutrition and Integrative Physiology at the University of Utah College of Health. “We were stunned—not only did kidney function stay normal, but the mitochondria were unscathed. It was truly remarkable.”
The study results also indicated that urine ceramides can predict disease severity in children and in adults. Summers is senior author of the team’s published paper in Cell Metabolism, titled “Therapeutic remodeling of the ceramide backbone prevents kidney injury,” in which they concluded “These studies describe a new, therapeutically tractable mechanism underlying PT mitochondrial damage in AKI.”
Acute kidney injury (AKI) is a prevalent and serious clinical event that increases one’s risk for chronic kidney disease (CKD), morbidity, and mortality,” the authors wrote. “The condition results from diverse insults including drug toxicity, sepsis, shock, heart failure, and pre-existing kidney conditions.” AKI also affects 20–30% of all patients undergoing cardiothoracic surgery. There are currently no drugs to treat AKI. “Given the substantial economic burden associated with AKI, as well as the lack of effective therapeutic options, identification of novel treatments to treat and prevent AKI is of critical clinical importance,” the team continued.
The Summers lab had previously shown that ceramides can damage different tissues, ranging from heart to liver. When the team profiled ceramides in models of AKI the correlation was striking, showing that ceramide levels spiked sharply after kidney injury in mice, and were elevated in human urine samples. The findings, they noted, “… demonstrate that humans and mice with AKI have dramatically altered renal ceramide metabolism, including induction of enzymes that drive de novo ceramide biosynthesis in PTs and pronounced ceramide accumulation in in tissue (mouse) or urine (human).”
“Ceramide levels are very elevated in kidney injury,” said first author Rebekah Nicholson, PhD, who carried out the research as a graduate student in nutrition and integrative physiology at U of U Health and is now a postdoctoral fellow at the Arc Institute. “They go up quickly after damage to the kidneys, and they go up in relation to the severity of the injury. The worse the kidney injury is, the higher the ceramide levels will be.” These findings suggest that urinary ceramide levels could serve as an early biomarker for AKI, helping doctors identify patients at risk—such as those undergoing heart surgery—before symptoms appear.
“Our identification of urine ceramides as candidate AKI biomarkers also has important clinical implications,” the investigators stated. “Current AKI diagnostics, including serum creatinine and urine output suffer from delayed kinetics, low sensitivity, and inability to capture subclinical disease… Our work suggests that urinary sphingolipid measurement could complement existing markers.” Nicholson added, “If patients are undergoing a procedure that we know puts them at high risk of AKI, then we can better predict whether or not they’re actually going to have one.”
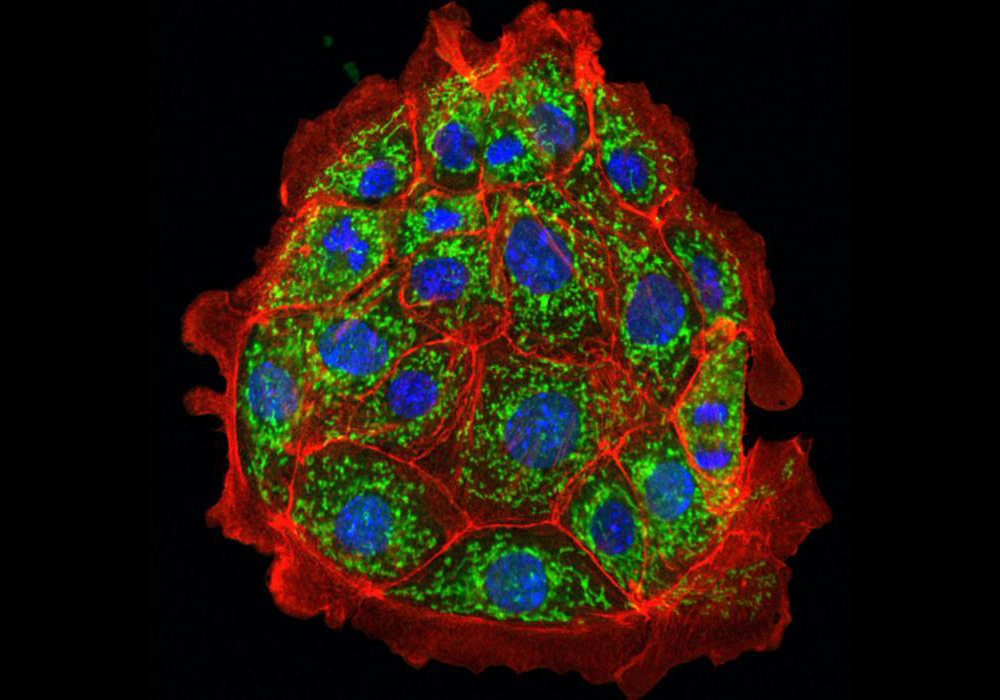
Ceramides cause kidney injury by damaging mitochondria, the part of the cell that produces energy, the researchers found. Mitochondria in injured kidney cells are visibly malformed under a microscope, and they can’t produce energy as efficiently. The researchers were able to almost completely prevent kidney injury in an animal model by changing how ceramides are produced. Mice engineered to lack a gene, DES1, involved in ceramide were protected from AKI, even under what would usually be triggering conditions. “Genetically ablating DES1 preserved mitochondrial integrity and prevented kidney injury in mice following bilateral ischemia reperfusion,” the researchers explained.
Similarly, kidney injury was also prevented in mice pretreated using a new ceramide-lowering drug candidate developed by Centaurus Therapeutics, a company co-founded by Summers. Kidney function improved, mice stayed fully active, and the kidneys looked nearly normal under the microscope. The model the researchers use tends to put the kidneys under a lot of stress, Nicholson said, so “it’s really remarkable that mice were protected from the injury.” Summers added, “These mice looked incredible.”
Summers emphasized that the compound used in the study is closely related to, but not the same as, the ceramide-lowering drug that has advanced into human clinical testing. Results in mice don’t always translate directly to humans, he noted, and additional studies are needed to establish safety.
“We’re thrilled by how protective this backup compound was, but it’s still preclinical,” Summers stated. “We need to be cautious and do our due diligence to make sure this approach is truly safe before moving it into patients.” The researchers are nevertheless optimistic. If the results hold true in humans, the researchers hope that the drug could be provided in advance to people at high risk of acute kidney injury—such as people undergoing heart surgery, about a quarter of whom experience AKI.
Because the drug seems to work by keeping mitochondria healthy, the researchers suspect that it might help treat or prevent many other diseases that affect mitochondria. “Mitochondrial problems show up in so many diseases—heart failure, diabetes, fatty liver disease,” Summers said “So if we can truly restore mitochondrial health, the implications could be enormous.”
In conclusion, the authors wrote, “… the study represents an important conceptual advance that informs about the role of ceramides in AKI, the value of urinary ceramides as biomarkers of kidney injury, the mechanisms that underlie the lipid’s actions on mitochondrial metabolism, and the potential of a new therapeutic approach for treating kidneys—or perhaps other tissues—exposed to ischemia reperfusion.”