Researchers at the Icahn School of Medicine at Mount Sinai have identified specific features of the immune system help explain why some patients with multiple myeloma (MM) experience long-term remission following CAR T cell therapy, while others relapse within a few years. The research, published in Blood Advances, focused on the BCMA-targeted therapy cilta-cel and found that long-term MM survival was linked to an interaction between the infused CAR T cells and a patient’s own immune system.
“CAR T cell therapy has changed myeloma care, but not everyone maintains a long remission,” said senior author Alessandro Lagana, PhD, assistant professor of oncological sciences at the Icahn School of Medicine at Mount Sinai. “We wanted to understand what’s happening in the immune system of patients who stay in remission for more than five years after a single infusion.”
The research is the first longitudinal, single-cell, multiomic study of cilta-cel (ciltacabtagene autoleucel) in MM. In this study, the Mount Sinai researchers analyzed 19 patients from the CARTITUDE-1 clinical trial, using blood and bone marrow samples collected before and after therapy to uncover how both infused and native immune cells evolve over time.
Their data showed that patients who remained cancer-free for more than five years had a focused, early expansion of CAR T cells and maintained a broad, diverse pool of endogenous CD4 helper T cells. Patients who relapsed had higher baseline tumor burden and early proliferation of suppressive myeloid-derived cells that likely hampered immune activity.
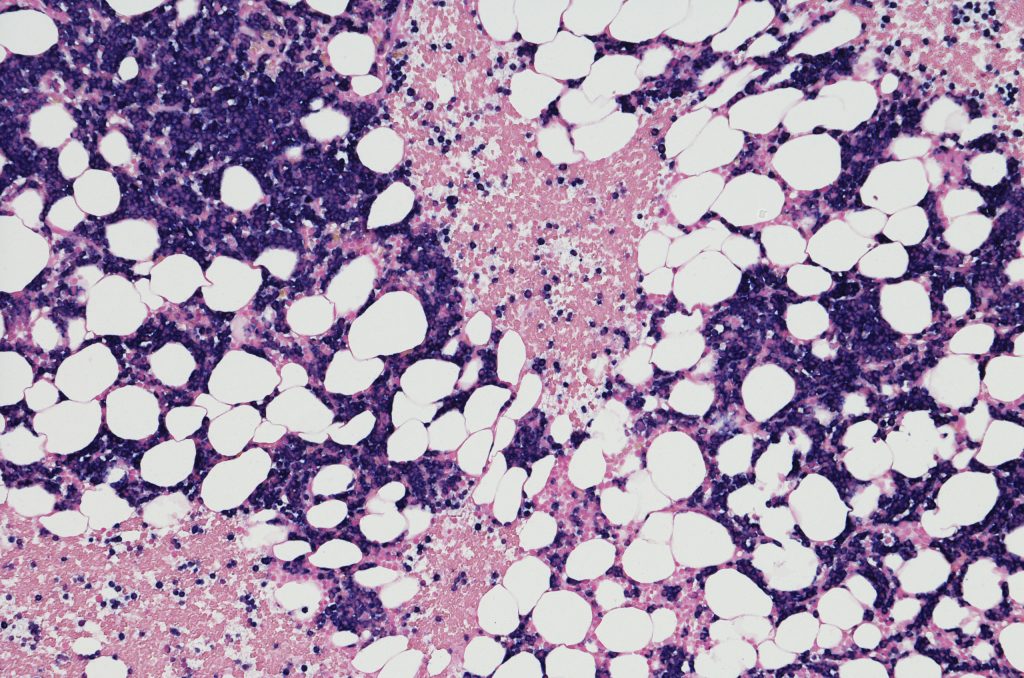
By comparing the immune features of patients who achieved progression-free survival (PFS) longer than five years with those who relapsed earlier, the study provides a detailed map of cellular and molecular signatures linked to durable remission. Bone marrow samples from patients who experienced an early relapse of disease had significantly higher plasma cell percentages at baseline (median 48% vs. 2%), which correlated with prior research showing the negative impact of high tumor burden on CAR T cell function and immune reconstitution.
T cell receptor sequencing of long-term responders revealed extensive immune remodeling post-infusion. “The combination of broad endogenous diversity and potent CAR T oligoclonality may reflect a synergistic immune landscape conducive to sustained tumor control,” the researchers wrote. This interplay suggests that durable disease control requires a balance between a potent CAR T response and a resilient, diverse native T cell repertoire.
The study also found broad immune environment differences between early-relapse patients and long-term responders after therapy. Those whose cancer relapsed within five years had strong negative correlations between myeloid-derived suppressor cells (MDSCs) and CD4-memory T cell subsets, which indicated that early expansion of suppressive myeloid cells may blunt T cell responses. Long-term responders, however, showed higher frequencies of naïve CD4 T cells at baseline and post-infusion increases in antigen-presenting monocytes, creating an environment that is potentially more favorable for sustained antitumor activity.
“This research shows that long remissions depend not only on the CAR T cells we give, but also on the patient’s own immune system,” Lagana said. “Understanding these immune patterns could help doctors choose the right patients for CAR T cell therapy, watch for early signs of relapse, and develop new treatments that keep the immune system strong and responsive.”
Prior data from the CARTITUDE-1 trial had shown that one-third of patients achieved progression-free survival of at least five years after a single cilta-cel infusion, but the biological reasons were not well understood. These new findings provide a mechanistic basis for these outcomes, and is comparable to earlier research in other hematologic cancers that link broad T cell recruitment and a healthy endogenous immune system with long-term response to CAR T therapy.
The Mount Sinai team believe these new findings can be use to help guide both patient selection as well as inform the development of new therapies. By identifying immune signatures predictive of durable remission, clinicians could potentially stratify patients before CAR T infusion or pursue other strategies aimed at strengthening immune recovery.
“Strategies to preserve or enhance endogenous T cell function, such as early intervention before extensive T cell depletion, use of immune rejuvenating agents, or integration with checkpoint blockade, may further enhance the efficacy of CAR T therapy,” the researchers wrote.
The researchers are now looking to test these findings in a larger cohort of patients and developing a new clinical assay that could measure a patient’s immune health before receiving CAR T therapy. Such a test could stratify patients into those most likely to benefit from CAR T immunotherapy from those who might benefit from interventions aimed at bolstering the immune system before receiving CAR T.