Researchers at ChristianaCare Gene Editing Institute have leveraged CRISPR gene editing to overcome chemotherapy resistance in lung cancer by disabling a tumor-specific mutation in the NRF2 gene, according to a recent study published in Molecular Therapy Oncology.
“NRF2 activation in cancer promotes resistance to chemotherapy and radiation, often driven by mutations in NRF2, like R34G, which is common in lung squamous cell carcinoma,” said the study’s lead author Kelly Banas, PhD, associate director of research at the Gene Editing Institute. “This mutation creates a unique CRISPR/Cas target site, enabling selective editing of cancer cells while sparing healthy ones.”
The NRF2 gene functions as a master regulator of genes that enable cancer cells to withstand chemotherapy, radiotherapy, and immunotherapy and has been studied by the team at the Gene Editing Institute for the past 10 years. The level of NRF2 in tumor cells is often a clear determinant of the effectiveness of standard of care treatments. When NRF2 becomes overactive, often through mutations that prevent its normal degradation, the protein accumulates, allowing tumor cells to evade cancer treatments.
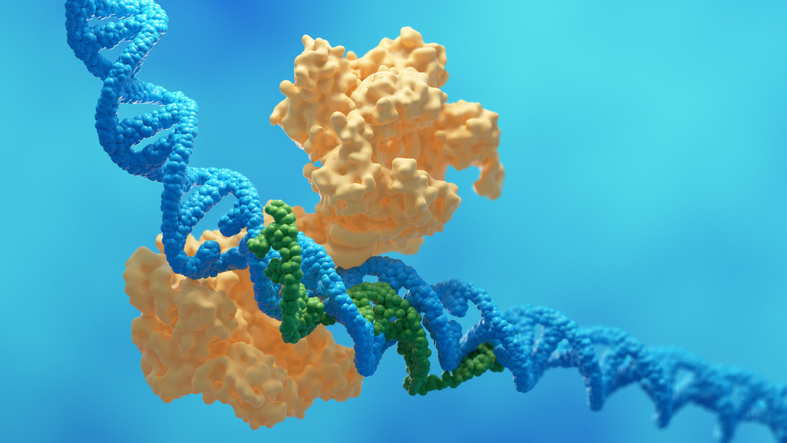
To develop their CRISPR-based therapeutic approach to overcome this resistance, the researchers targeted the R34G mutation because of its prevalence in lung squamous cell carcinoma, which creates a unique CRISPR/Cas9 cleavage site. “The appearance of this new protospacer adjacent motif (PAM) site affords the opportunity for the CRISPR-Cas complex to cleave the mutated NRF2 genome while leaving the wild-type genome intact,” the researchers noted in their paper. This allowed CRISPR to selectively disrupt NRF2 in tumor cells and chemosensitivity without altering effects on healthy tissue.
Earlier attempts to target NRF2 with drugs were not effective, according to Banas. “What has been interesting about NRF2 as a target is that drugs that both activate and deactivate the protein have proven to be only mildly successful. Our decade long research using gene editing on NRF2 has led us to understand that a critical reduction of NRF2 needs to be reached in cancer cells to induce a response, and the most effective way to do so is to disrupt NRF2 on the gene level using CRISPR.”
To test their approach, researcher engineered human lung cancer cell lines with the R34G mutation and disrupted NRF2 using CRISPR/Cas9. They assessed genomic, transcriptomic, proteomic, and phenotypic changes to determine the effects of this gene editing on drug response.
The data showed that knocking out NRF2 restored sensitivity to chemotherapy agents such as carboplatin and paclitaxel and loss of NRF2 protein correlated with decreased expression of its target genes, including NQO1, HMOX1, and GCLC, which demonstrated that the targeted CRISPR editing disrupted NRF2-driven survival pathways.
“The surprising finding was that complete gene editing in the tumors wasn’t necessary to see an effect with and without the combination of chemotherapy—suggesting a threshold level of NRF2 that needs to be knocked out for tumors to respond,” said Banas. In both the lung cancer cell line and animal model testing, the results showed that editing just 20% to 40% of the tumor cell population was enough to resensitize tumors to treatment.
Although the study centered on lung squamous cell carcinoma, overactive NRF2 contributes to treatment resistance in several solid tumors, including liver, esophageal, and head and neck cancers. So there is potential broader use for a CRISPR-based NRF2-targeting approach.
The findings also suggest that NRF2 editing might have value not only after resistance develops but potentially earlier in treatment. “Because NRF2 helps cancer cells resist stress, knocking it out at any stage could improve effectiveness of standard treatments and might even prevent resistance from developing when used early,” Banas noted.
Based on these results, the Gene Editing Institute team is now preparing for the regulatory steps required to move the therapy toward clinical trials. “The team has completed proof-of-concept work and assembled all the components necessary for a pre-IND submission—delivery strategy, in vitro and in vivo validation, and off target analysis,” Banas said. CorriXR Therapeutics is advancing the therapeutic candidate through the FDA approval process with the goal of reaching lung cancer patients.
Should it be approved, the researchers noted that CRISPR would augment current therapy approaches and not replace them. “Our work has always assumed that CRISPR-Cas would be used as an augmentative therapy to support standard of care by facilitating the disruption of genes causing resistance or reducing effective sustainability of targeted therapies,” the investigators wrote. “Strategically, we feel that by lowering the amount of chemotherapy needed to inhibit tumor growth, a patient will be able to tolerate treatment for longer periods of time supporting more beneficial outcomes.”