Researchers at the University of Cambridge have developed an artificial intelligence (AI) model named CytoDiffusion that can analyze blood cells in a patient sample with more accuracy and reliability than trained clinicians. Results published today in Nature Machine Intelligence show this technology has the potential to improve the diagnosis of a wide range of conditions affecting blood cells while reducing time doctors spent in routine tasks.
From anemia to cancer, a wide range of blood disorders can be diagnosed using a blood smear test, where a hematology specialist observes the size, shape and number of blood cells in a patient sample under the microscope. “Knowing what an unusual or diseased blood cell looks like under a microscope is an important part of diagnosing many diseases,” said Simon Deltadahl, PhD candidate at the University of Cambridge and first author of the study.
However, years of training are required to accurately pick up on subtle differences between blood cells that may indicate disease, and experts may not always agree on the interpretation of some of the more challenging cases. While there are computer tools available to support doctors on this task, conventional machine learning methods struggle to accurately identify blood cells due partly to the high variability seen between blood cells in a sample as well as between patients.
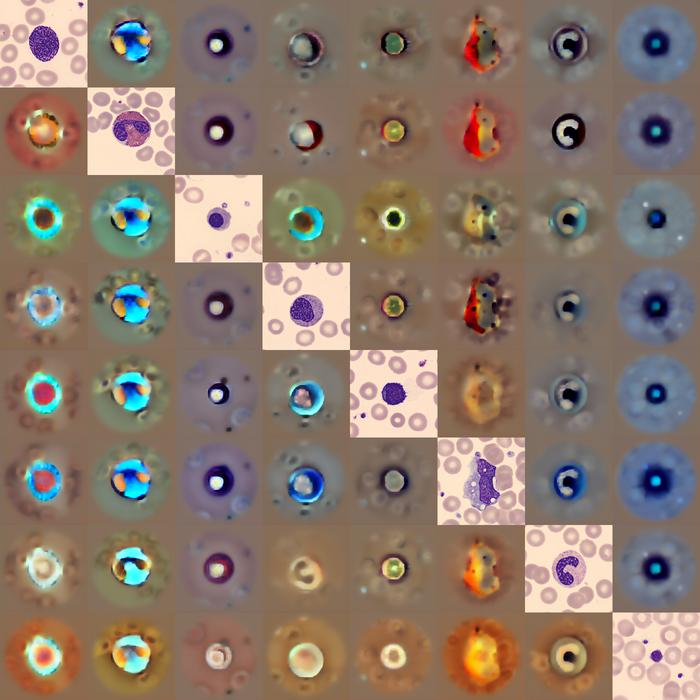
To overcome these limitations, Deltadahl and colleagues developed CytoDiffusion using a diffusion-based generative model, a type of AI algorithm commonly used for image and video generation. Compared to the simpler classification algorithms used in conventional AI models, this algorithm is better at modeling complex visual patterns and can learn to model the full range of variability seen in blood cell shapes.
The resulting model was shown to accurately analyze all cells in a blood smear, which amounts to thousands of individual cells in each sample. “Humans can’t look at all the cells in a smear—it’s just not possible,” said Deltadahl. “Our model can automate that process, triage the routine cases, and highlight anything unusual for human review.”
When looking for abnormal blood cells, CytoDiffusion showed over 90% sensitivity and 96% specificity, consistently outperforming other state-of-the-art machine learning models. To ensure robustness, the team tested the model against real-world AI challenges such as images it has never seen before and images captured using different equipment. In addition, the model was able to generate synthetic images of blood cells that expert hematologists could not distinguish from real images.
“When we tested its accuracy, the system was slightly better than humans,” said Deltadahl. “But where it really stood out was in knowing when it was uncertain. Our model would never say it was certain and then be wrong, but that is something that humans sometimes do.”
“Our work suggests that generative AI will be central to this mission, transforming not only the fidelity of clinical support systems but their insight into the limits of their own knowledge,” said Parashkev Nachev, PhD, professor of neurology at University College London. “This ‘metacognitive’ awareness—knowing what one does not know—is critical to clinical decision-making, and here we show machines may be better at it than we are.”
The AI was trained with data from over half a million images of blood smear tests performed at Addenbrooke’s Hospital in Cambridge, making it the largest dataset of its kind. The researchers are making this dataset publicly available for the scientific community. “By making this resource open, we hope to empower researchers worldwide to build and test new AI models, democratize access to high-quality medical data, and ultimately contribute to better patient care,” said Deltadahl.
The research team stressed that this model is not meant to replace trained clinicians. Rather, it has been designed to support them by flagging abnormal cases while handling the more routine tasks. “The true value of healthcare AI lies not in approximating human expertise at lower cost, but in enabling greater diagnostic, prognostic, and prescriptive power than either experts or simple statistical models can achieve,” said Nachev.