Researchers at the University of Texas MD Anderson Cancer Center report that heat shock protein 90 (HSP90) plays a previously unrecognized role in BRCA1-driven breast cancers by buffering a number of BRCA1 mutations, masking their negative effects and delaying cancer onset. The research, published in Molecular Cell, shows that this buffering by HSP90 creates vulnerability in cancer cells and that targeting the protein could be a therapeutic approach to overcome treatment resistance.
“Mutations are not all the same. Understanding the mechanisms that distinguish them can improve our ability to predict clinical outcomes and to target mutations more effectively in patients,” said senior author Georgios Karras, PhD, an associate professor of genetics at MD Anderson.
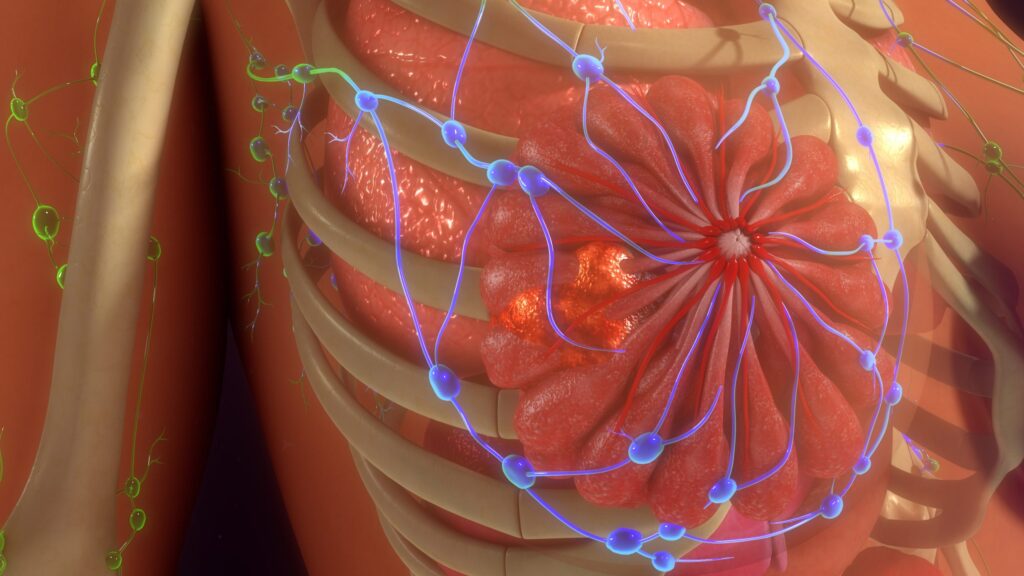
The discovery of the effects of HSP90 was produced by a series of cellular experiments designed to define how HSP90 interacts with BRCA1 variants in the BRCT domain, a genetic hotspot for cancer causing mutations. The researchers noted that “HSP90-buffered BRCA1-BRCT variants retain physiological interactions with partners and support cell fitness but show increased dependence on HSP90 for their stability.” In total, the researchers estimated that 18% of known BRCA-BRCT missense mutations are buffered by HSP90.
By analyzing how BRCA1 mutants folded, interacted with protein partners, and responded to stress, the researchers found that many of the BRCA1 variants depend strongly on HSP90 to maintain their stability and function in cell survival.
Earlier research unrelated to cancer had shown HSP90 playing a similar role of buffering genetic variation in diverse organisms, and this activity could modify disease presentation. However, its role in common cancer-driving genes was not known. “HSP90 buffers genetic variation across diverse organisms, thereby altering the course of evolutionary processes,” the researchers wrote, while adding that that other studies of protein-folding biology suggested many pathogenic missense mutations destabilize proteins. The researchers sought to find if this also applied to BRCA1 and discovered that buffering of human cancer-predisposition mutations is more prevalent and clinically significant than was previously known.
For their study, the MD Anderson team ran high-throughput functional assays of BRCA1-BRCT missense variants, mapped HSP90 binding characteristics, and tested the impact of environmental stress on protein stability. They also examined clinical data to evaluate cancer onset in patients carrying HSP90-buffered mutations.
An important discovery of this research was that HSP90 buffering promotes resistance to PARP inhibitors and noted the following:
- HSP90 buffers certain BRCA1 mutations, allowing them to persist in humans and promote resistance to PARP inhibitor treatments;
- Low-dose HSP90 inhibition restored PARP inhibitor sensitivity in HSP90-buffered BRCA1-mutant cells; and
- Researchers identified specific features of HSP90 buffering to find patients most likely to benefit from a combination therapy targeting HSP90
Analysis of patient data showed that HSP90 buffering delayed breast cancer onset by about a decade, a finding that could influence patient counseling and risk-management decisions. This suggests “that premenopausal carriers of HSP90-buffered BRCA1 mutations might not benefit from prophylactic mastectomies,” the researchers wrote.
For clinical applications, this research identified predictive features of HSP90 buffering in patients with specific mutations in BRCA1 that could guide clinicians to develop individualized diagnosis, prognosis, and identify combination treatments. The researchers hypothesized that one such approach to improve treatments would be low-dose inhibition of HSP90 to help enhance response to PARP inhibitors, noting that HSP90 buffering could be responsible for a significant proportion of breast cancer cases that are resistant to PARP inhibition.