“I’ll end with a little bit of a wild, crazy idea, but I think it’s actually one that has the real potential for the benefit of patients.”
The room was stunned when David Liu, PhD, the inventor of the genomic keyboard from base editing and prime editing, said this two-thirds of the way through his February talk at the Precision Medicine World Conference (PMWC) 2025 in Silicon Valley. The entire audience, including those on their phones, became laser-focused on the speaker and screen, in an anticipatory freeze, until Liu revealed that his lab was developing single gene-editing therapies to treat multiple, unrelated genetic diseases regardless of gene or tissue.
It wasn’t until months later when Liu joined me on the Behind the Breakthroughs podcast that I got another sneak peek. In the episode, Liu explained that “one composition of matter, one syringe of stuff”—one prime editing agent plus one pegRNA—could permanently treat multiple patients with unrelated genetic diseases. He teased that his lab had exciting results with a publication due later in the year. That left me waiting for the next clue, which finally materialized this week.
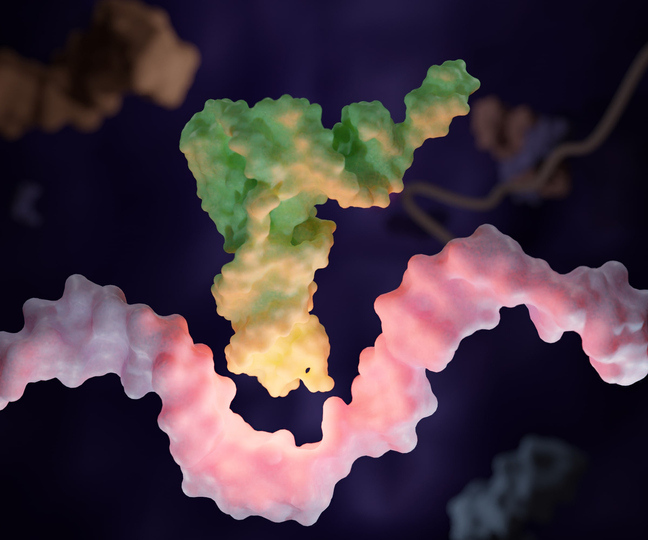
The “wild, crazy idea” Liu was referring to is called prime editing-mediated readthrough of premature termination codons (PERT), a strategy to rescue nonsense mutations in a “disease-agnostic” manner. PERT uses a single prime editing composition to permanently convert a “dispensable” endogenous tRNA into an optimized suppressor tRNA (sup-tRNA) that reads through a premature stop codon.
The article published in Nature shows that simply changing one building block of DNA to create a permanent suppressor tRNA, instead of fixing a faulty gene, could potentially help treat many stop codon disorders. Premature stop codons—which result in truncated proteins—occur in roughly 10–15% of pathogenic variants and contribute to nearly a third of known Mendelian disorders.
“Once you’ve developed and optimized one prime editor that can install a tRNA that can rescue a certain type of premature stop codon, you may be able to apply that same prime editor to many different premature stop codons in the same gene or in other genes,” Liu told Inside Precision Medicine this week. “This strategy could dramatically reduce the time and cost of developing treatments for patients whose individual mutations are too rare to justify bespoke programs. Delivery will still need to be tailored to each tissue—the eye versus the muscle versus the liver versus the blood—but the editor itself could remain the same. The editing can be developed in a way that’s not just mutation agnostic but, in some respects, also disease agnostic.”
As the field looks beyond single-mutation therapies toward platforms that could help far larger patient populations, researchers see a convergence of interests across science, industry, and regulation. “Everyone’s interests and the way we see what’s needed for the future to get the promise of gene editing treatments to benefit as many patients who urgently need these treatments as possible are all pointing in the same direction,” Liu said.
Nonsense mutation therapeutics reimagined
Therapeutic strategies for nonsense mutations include small-molecule readthrough drugs, gene therapy, and engineered suppressor tRNAs, each with distinct advantages and limitations. Readthrough drugs are simplest—coaxing ribosomes to ignore premature stops—but offer modest protein rescue, require lifelong dosing, and act inconsistently. Gene therapy, typically via adeno-associated viruses (AAVs), supplies a new gene but is gene-specific, limited by vector size, and affected by durability and immune barriers. Engineered suppressor tRNAs, such as those developed by Alltrna, are more gene- and disease-agnostic, yet as macromolecules they face challenges in potency, specificity, and dosing.
Dan Wang, PhD, assistant professor at UMass Chan Medical School, whose lab works on AAV gene therapy and previously developed small-molecule readthrough agents, explained that while these drugs can, in principle, reach the whole body, they have major drawbacks—especially in multisystem disorders like Hurler syndrome (MPS I), caused by a nonsense mutation in IDUA that leads to widespread glycosaminoglycan accumulation.
Because effective readthrough drugs require high dosing, Wang described “a dilemma—you want to reach as many body parts as possible, but in other cases you want to specifically target the place you want to target.” Tissue sensitivity complicates this further: neurons may be more sensitive to global readthrough toxicity, Wang says. For muscle- or liver-focused diseases, “you do not want your agent to go as many places as possible—you want to target the tissues that really matter.”
Wang noted that all these approaches share a common safety concern: off-target effects on normal stop codons. “This issue still needs to be studied in larger animals and over longer time frames to fully assess the safety profile of read-through agents, whether small molecules or other modalities.” A few such studies exist—he has seen at least one conference abstract—but research is ongoing.
Liu’s team at the Broad Institute tackled nonsense mutations using prime editing to convert redundant tRNA genes into sup-tRNAs. Humans have 418 high-confidence tRNA genes but only need 61 codons, leaving many dispensable. Evidence shows people with deletions or anticodon-altering mutations in certain tRNAs remain healthy, and cellular systems like redundant termination signals and nonstop decay protect against errors.
Postdocs Sarah Pierce, PhD, and Steven Erwood, PhD, systematically converted all 418 human tRNA genes into candidate suppressors. Early versions were weak: one endogenous copy usually produced weak read-through, prompting libraries of anticodon variants, leaders, terminators, and base-pair modifications. This yielded “super-suppressor” tRNAs producing full-length proteins roughly fivefold higher than anticodon-only designs. Optimized leucine-specific sup-tRNAs, plus arginine, tyrosine, and serine backbones, restored up to 35% of normal GFP in reporter assays.
Prime editing installed these suppressors at endogenous loci with 70–80% efficiency. A single editor rescued three nonsense mutations in human cell line models of unrelated genetic disorders—Batten disease, Tay–Sachs disease, and cystic fibrosis—restoring 20–70% of normal enzyme or protein levels. In vivo, a GFP reporter mouse showed 10–20% editing and ~25% normal GFP across brain hemispheres. In a Hurler syndrome model, the same editor delivered by AAV restored 5–7% of normal enzyme activity across multiple tissues—above the ~1% needed for full rescue—and treated mice showed near-complete correction of symptoms.
The off-target problem (and other safety concerns)
Liu’s team also tested whether their approach might inadvertently disrupt cells. One concern was off-target editing. As others have reported, prime editing generally yields very low off-target activity because its multi-step mechanism creates multiple checkpoints that reject incorrect matches. Using two complementary, genome-wide detection assays—methods the researchers developed specifically to be unusually comprehensive—they found no detectable off-target edits when replacing the endogenous tRNA with the optimized TAG-suppressor tRNA.
Another potential risk was unintended read-through of natural stop codons. More than 4,000 human genes end with a TAG termination codon, and bypassing those stops could generate aberrant proteins. To seek evidence, Liu’s team calculated the exact peptides that would be produced if translation ran past the natural TAG and into the 3′ UTR, then searched for them using targeted mass spectrometry. As a positive control, they confirmed abundant read-through peptides from the engineered GFP reporter. However, Liu was surprised that his team did not find any peptides that corresponded to read-throughs at native TAG stop codons. The only gene that produced a faint signal was YARS, which encodes tyrosyl-tRNA synthetase, but the amounts were so low that they were not deemed statistically significant.
“Somewhat to my surprise, we did not observe a single peptide corresponding to readthrough of the natural termination codon at protein-coding sequences that are naturally terminated with tag stop codons,” said Liu. “We observed one signal that might be a real signal at a very low level, but it was statistically significant compared to the untreated control.”
Finally, the researchers measured global RNA and protein levels, a sensitive way to spot cellular stress or other unintended perturbations. Liu explained dramatic changes in the stoichiometry of the components of translation—that is, sudden increases in the concentrations of a tRNA by a factor of 10, 100, or 1,000, or changes in the concentration of amino acids by large amounts—can globally perturb translation.
“Changing the stoichiometry of the components of translation can cause translation to speed up or slow down for different transcripts. You can even cause the quality control, that is, the accuracy of translation, to get eroded,” said Liu. “This phenomenon has been known for decades. If you flood a cell with one type of tRNA, you can observe more mistakes in which that tRNA inserts its amino acid, even if the codon isn’t a perfect match for the anticodon of that tRNA. Because translation, like many complicated processes in biology, is really a competition between dozens of different molecules.”
Contrary to Liu’s predictions, the research team saw no transcripts or proteins that changed by more than twofold between treated and untreated cells, a common threshold for meaningful biological effects.
Taken together—the absence of detectable off-target edits, stop-codon read-through, or shifts in the transcriptome and proteome—suggests the system leaves the cell’s natural state largely undisturbed. Still, the researchers emphasized that negative results are limited by the sensitivity of the methods used. Consummate scientist that he is, Liu said, “All negative results have to be viewed through the lens of the method used to detect them. While we did our best to use state-of-the-art methods to detect each of those kinds of potential unwanted consequences, all we can say is that the methods we use did not lead to detected off-target edits or translation past natural termination codons or changes in the transcriptome and proteome.”
Beyond stop codon diseases
Erwood explained that the Broad team chose to convert an endogenous tRNA into a suppressor to keep the system “as minimally disruptive as possible” and to maintain native regulation. “In this first demonstration, we took a relatively simple approach: we used prime editing to rewrite an endogenous tRNA gene into a sup-tRNA,” Erwood told Inside Precision Medicine.
“That worked well for our chosen leucine tRNA locus, which was safely ‘repurposeable.’ But that won’t always be the case… imagine you identify a very potent arginine suppressor tRNA, but the endogenous arginine tRNA gene that encodes it can’t be safely rewritten without disrupting normal translation.”
Editing efficiency, delivery, and the context of the specific premature stop codon will also matter. “Some contexts are easier to suppress than others, as we’ve already seen when we tested PERT against a handful and then thousands of premature stop codons,” said Liu. “Next, we’re expanding PERT by expanding the scope of the termination codon and the amino acid that can be installed.”
Liu hopes to build a toolkit that can handle all variations of nonsense mutation. “We would like to assemble… a small set of PERT agents for each stop codon so that you have the choice of a few different flavors of amino acid… maybe a hydrophobic one, a positively charged one, a negatively charged one, and a polar one,” he said. “If you had a dozen such flavors, there would be a reasonably high chance of being able to functionally rescue just about any premature stop codon.”
In speaking with Inside Precision Medicine, Pierce noted that the backbones identified so far could “correct >30% of all documented nonsense mutations with precise installation of the original amino acid.” Because “only 19 single nucleotide changes lead to a nonsense mutation,” she added, “we would only need to optimize 19 different sup-tRNA backbones… for precise correction of all nonsense mutations with PERT.”
In principle, the suppressor tRNA could also be delivered from a designed promoter–terminator cassette inserted into a genomic safe harbor using twin-PE, PASSIGE, or EvoCAST. “Tools like twinPE or eePASSIGE would let you install a new suppressor tRNA cassette elsewhere in the genome while preserving expression of the original arginine tRNA gene,” Erwood said. This approach would also allow inclusion of suppression-enhancing variants not feasible when rewriting an endogenous tRNA directly.
“In theory, you could achieve PERT without converting an endogenous, dispensable tRNA… just by adding the engineered suppressor to the genome,” Liu said. “personally, I think it’s particularly elegant to convert one of the 418 tRNA genes… because it seems less perturbative… than adding something into a cell and not knowing if the place that you added is going to get chromatinized or regulated in a way that you didn’t anticipate.”
Pierce added that for tRNA families with high sequence similarity, installing the suppressor elsewhere “would allow us to safely install that sup-tRNA without targeting an entire family of tRNA genes at once.”
Liu is also considering how these insights might apply to other shared molecular defects. “We’re also trying to expand the same approach to cover other types of common information-flow abnormalities,” he said. “For example, quite a few diseases are caused by misfolding or mislocalization of proteins.” Many genetic disorders converge on such shared pathways, making them attractive targets for broadly applicable therapies.
Speeding up regulatory approval
Despite their promise, sup-tRNAs face major hurdles. Ensuring safety while altering fundamental translational or RNA-processing machinery is nontrivial, as broad-acting interventions risk unintended off-target consequences. Delivery remains another challenge: a truly gene-agnostic therapy must work in multiple tissues, some of which are difficult to reach.
Liu points to “Baby KJ,” whose case marked the first clinical use of CRISPR base editing. One of the two disease-causing mutations he inherited was a TAG stop codon—exactly the type PERT is designed to bypass. “There are lots of other premature TAG stop codons in liver diseases that cause serious disease,” Liu noted. In such settings, where delivery technologies like AAV or LNPs are already clinically validated, “you don’t need to invent any new science or delivery or manufacturing methods” to begin adapting those systems for PERT, once preclinical safety work is complete. “I don’t mean to imply that you should go put PERT into a patient tomorrow,” he added, “but… you may not need to invent much else.”
Progress in one tissue often accelerates progress across the board. The success of KJ’s treatment, Liu said, “has a synergistic impact,” de-risking future editing trials in the liver and beyond. The same dynamic may unfold with AAV-delivered editing agents, which build on decades of AAV-delivered gene-therapy experience. And with each new frontier crossed, the investment climate shifts. “the first successes will open up new opportunities,” Liu said, “additional organ systems could become viable targets for the next wave of programmable therapeutics.”
Regulatory pathways are still evolving for therapeutics that target a mechanism rather than a disease. If successful, gene-agnostic therapeutics could dramatically streamline the treatment landscape—allowing one composition of matter to address dozens of rare diseases at once. For patients with ultra-rare or underserved conditions, this shift could be transformative, offering a route to therapy that does not require bespoke drug development for each individual mutation.
Prime real estate
When Liu first teased the idea nine months ago, I imagined it was going to be something from another dimension. That didn’t end up being the case, as the idea of targeting premature stop codons created by nonsense mutations is decades old. Although absolute novelty was not the case, there has yet to be a clinically approved commercial product targeting stop codon diseases, which are remarkably prevalent. In the United States, around 8,000 people with cystic fibrosis, 252,000 with Stargardt disease, 31,000 with phenylketonuria (PKU), and 43,500 with Duchenne muscular dystrophy have specific gene changes that could potentially be treated with therapies aimed at fixing these types of mutations.
“To my knowledge, this seems to be the only available gene therapeutic approach that is disease-agnostic,” said Wang. “Typically, we take one disease and one therapy approach. For a defective gene, we have to deliver that gene for treating that particular disease; that’s it. And for gene editing, it’s even more specific; it’s allele- or mutation-specific in many cases.”
The larger question now is how such a platform could move from the lab into the clinic—and who would shepherd it there. PERT is still early-stage science, but its architecture naturally aligns with commercial development. A disease- and gene-agnostic therapy that uses the same editor and only swaps out the pegRNA or suppressor backbone resembles a true platform technology, one that could amortize development costs across dozens of indications. If the editor itself doesn’t change, much of the safety, delivery, and manufacturing work could, in principle, be reused, lowering barriers for ultra-rare diseases that currently have no market justification.
Whether PERT ultimately falls under the umbrella of Prime Medicine—the company Liu co-founded to translate prime editing technologies—remains an open question. The IP landscape surrounding prime editing is already tightly interwoven among Harvard, the Broad Institute, and Prime Medicine, and any therapeutic built on prime editing’s core components would almost certainly intersect with that estate.
Still, whether PERT becomes a Prime Medicine program or a new venture, the broader implications remain the same: a single composition of matter that could serve as the backbone for dozens of rare-disease therapeutics would mark a fundamental shift in how genetic medicines are developed, regulated, and commercialized. For patients whose mutations have long been too rare to interest industry, a platform like PERT could finally make them visible—not one mutation at a time, but all at once.