An analysis of prior research published in Nature Reviews Endocrinology has identified estrone, the dominant estrogen present in women after menopause, as the key driver of the inflammation, tumor progression, and metastasis of estrogen receptor–positive (ER+) breast cancer in postmenopausal women with obesity. The analysis describes how estrone that is produced in adipose tissue may create a tumor-promoting environment that differs significantly from the effects of premenopausal 17β-estradiol.
According to lead author Joyce Slingerland, MD, PhD, co-leader of the Cancer Host Interaction Program at Georgetown University’s Lombardi Comprehensive Cancer Center, estrone’s emergence as the primary estrogen after menopause is central to understanding why ER+ breast cancer incidence and mortality rise with age. Before menopause, the hormone 17β-estradiol is produced by the ovaries and exerts anti-inflammatory effects. But after menopause, its levels decrease significantly, making estrone the most abundant estrogen in blood, breast, adipose, and other tissues. Slingerland’s noted that estrone synthesized in adipose tissue becomes further elevated with increasing fat mass. In the context of obesity, levels of estrone are two- to four-fold higher in fat, breast, and other tissues, levels that “propel intense inflammatory activity,” the authors noted.
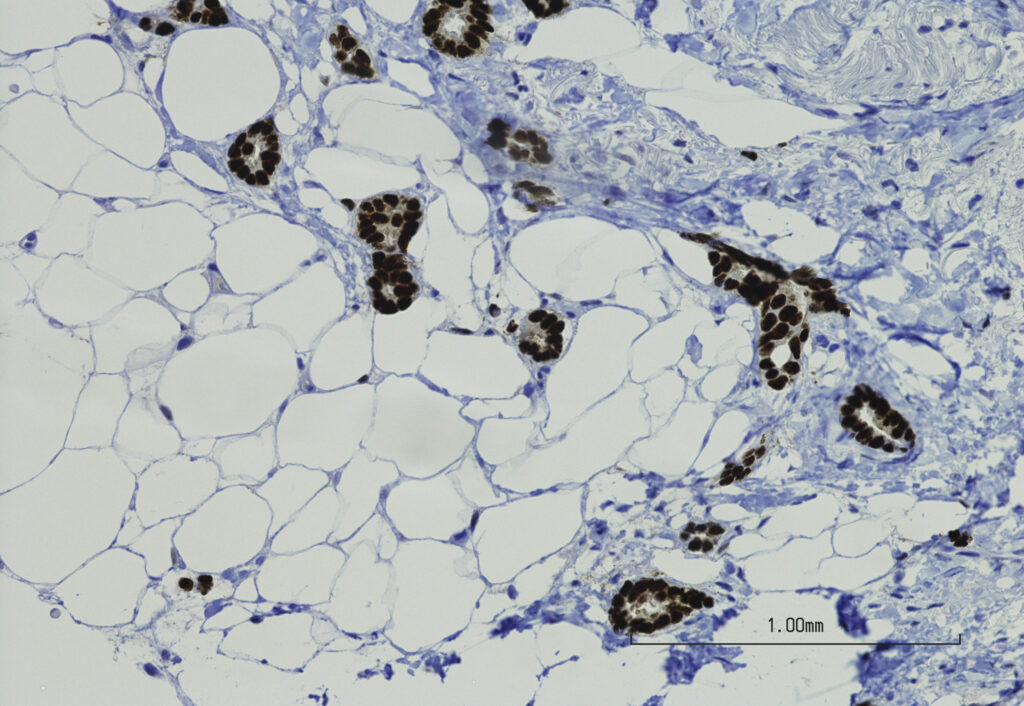
“Adipose tissue is chronically inflamed in obesity owing to pre-adipocyte expansion and activation of nuclear factor-κB (NF-κB), which upregulate pro-inflammatory cytokines. Obesity also impairs immunosurveillance,” the researchers wrote. Emerging evidence, they continued, shows that “the dominant postmenopausal estrogen, estrone, is pro-inflammatory. Estrone is synthesized in adipocytes, therefore the expanded adipose tissue biomass in obesity increases estrone levels…promoting NF-κB-driven inflammation.”
This shift from anti-inflammatory 17β-estradiol to pro-inflammatory estrone after menopause could offer and explanation as to why the majority of ER+ breast cancers arise in older women despite the decline in overall estrogen levels. In fact, ER+ cancers account for more than 70% of breast cancers in women over 70, with both the incidence and mortality rates rising after menopause.
The authors contend that estrone’s role has been understudied despite it being the dominant estrogen after menopause.
Slingerland’s prior work has shown that estrone works in conjunctions with NF-κB to activate pro-inflammatory cytokines, expand stem-like cancer cells, and stimulate invasive behavior. In a 2022 study published in Cell Reports, Slingerland and colleagues showed that estrone plays a role in promoting metastasis by activating epithelial-mesenchymal transition (EMT) gene programs. In that study, estrone was shown to accelerate tumor growth and caused rapid metastasis in ER+ breast cancer mouse models.
The new analysis suggests that this mechanism is more prominent in postmenopausal women with obesity. Their greater mass of adipose tissue fuels the production of estrone, and chronic inflammation further enhances the adipocyte-cancer cell interactions that promote tumor progression.
“High mammary adipocyte E1 synthesis and chronic inflammation in obesity would not only drive tumorigenesis but also the acquisition of mesenchymal invasive features, promoting local invasion and subsequent metastasis,” the authors wrote. These mechanisms align closely with findings from the 2022 Cell Reports study, which showed that intratumoral expression of the estradiol-to-estrone converting enzyme HSD17B14 accelerated metastasis.
The authors concluded that the hormonal transition at menopause—loss of estradiol and rise of estrone—combined with the higher estrone levels in obesity “might underlie the rise in ER+ breast cancer after menopause and its excess risk and mortality in those with obesity.” They suggest further research could focus on developing a better understanding of the enzymes that regulate estrone and estradiol.
There are some clinical implications of these findings. The evidence linking estrone to ER+ breast cancer “should prompt us to rethink how we approach treating cancer in these women,” Slingerland said. Because estrone is produced in adipose tissue, weight-loss interventions may help reduce its pro-inflammatory effects, which provides an opportunity to test weight lost drugs such as GLP-1 receptor agonists and dual GLP-1/GIP agonists as adjuncts to ER+ breast cancer therapy. “The GLP-1 drugs have revolutionized weight loss,” Slingerland noted. “Because of estrone’s powerful inflammatory effects in fat, there’s real potential that, by inducing weight loss, GLP-1 drugs can pump the brakes on estrone’s cancer-fueling behavior.”