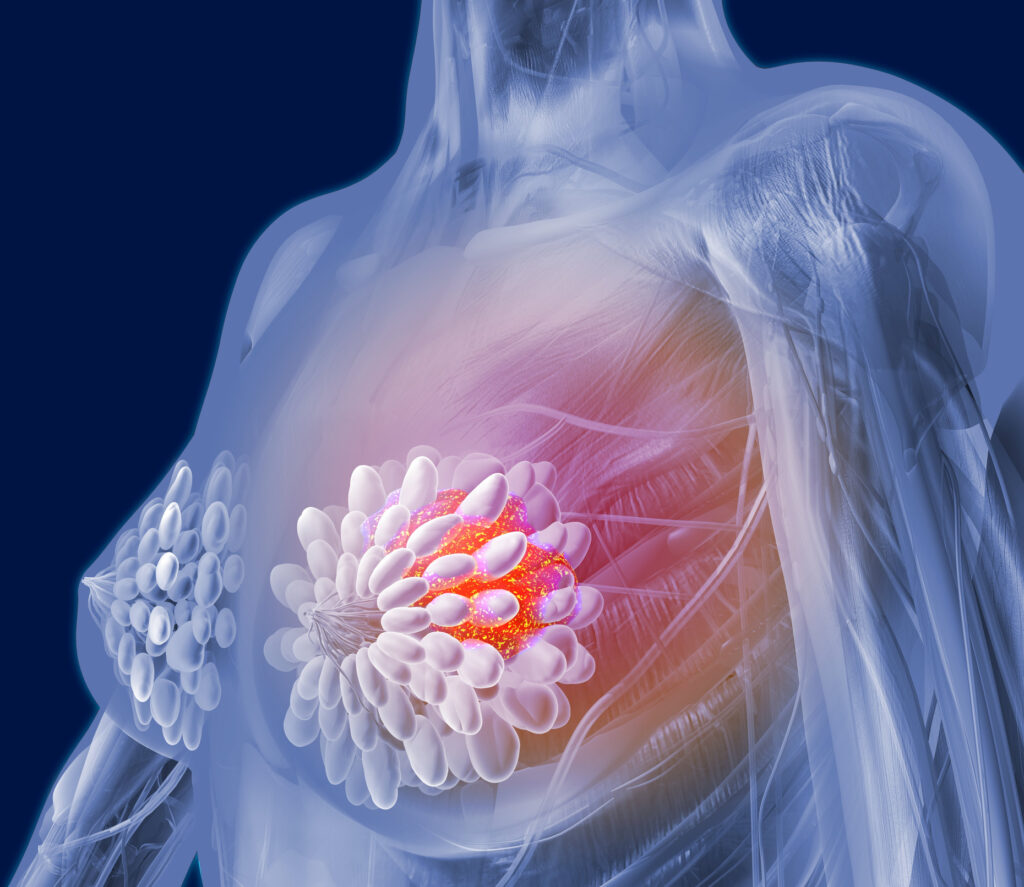
Results from an international research study suggest that women who carry either the BRCA1 or BRCA2 cancer-associated genetic mutations do not experience additional cancer risk if prescribed menopausal hormone therapy.
In a study including 1,352 women in menopause carrying these genetic variants, half were treated with hormone replacement therapy (HRT) and half were not. No increase in cancer risk in the HRT group was seen after almost six years of follow-up.
Millions of women experience the symptoms of menopause each year, yet effective treatment options remain limited. HRT has long been the primary approach to alleviating these symptoms, but its use declined sharply two decades ago following concerns about potential health risks.
This drop in HRT came about because findings from the Women’s Health Initiative (WHI) trials in 2002 suggested that HRT in healthy postmenopausal women carried more risks than benefits, including an increased likelihood of blood clots, strokes, and breast cancer. The results sent shockwaves through the pharmaceutical and medical communities, prompting a steep drop in HRT prescriptions.
While these results have since been questioned, new evidence shows that many women can benefit significantly from HRT when appropriately prescribed, there has still been a lot of caution around women in specific risk groups such as those know to carry cancer-associated variants like BRCA1/2.
The current study, presented at the San Antonio Breast Cancer Symposium by Joanne Kotsopoulos, PhD, a professor at the Dalla Lana School of Public Health at the University of Toronto, was initiated to try and assess the potential risks associated with HRT in menopausal BRCA1/2 variant carriers, many of whom undergo early menopause after having their ovaries removed to prevent ovarian cancer.
“Unfortunately, there has been a lot of reluctance and misinformation regarding menopausal hormone therapy, which is mostly attributable to findings from studies conducted in the general population,” said Kotsopoulos in a press statement.
“To help manage the side effects of oophorectomy safely in women with BRCA mutations, we need data from well-designed observational studies of menopausal hormone therapy use in this specific population who, due to their genetics, face elevated risks of breast cancer.”
For the current study, Kotsopoulos and colleagues recruited 676 menopausal BRCA1/2 variant carriers and the same number of menopausal controls with the same genetic variants who were matched by gene, year of birth and age at menopause.
After 5.6 years of follow up, there were actually more cases of breast cancer in the group who were not exposed to HRT than the HRT group at 128 (19%) versus 87 (13%) cases, respectively.
The researchers also looked at the type of HRT to assess if specific types had different effects. Most types of HRT showed no significant difference in breast cancer risk between the two groups, but there was an apparent protective effect observed in women taking estrogen. These women had a 63% lower risk for developing breast cancer during the follow up period than women with these mutations who were not exposed to HRT.
The type of genetic variant did not seem to significantly influence the results with similar outcomes seen in women with BRCA1 and BRCA2 variants.
“These findings provide an evidence-based approach for the management of women at high-risk of breast cancer who are facing the acute and chronic effects of early surgical menopause,” conclude Kotsopoulos and team.