Researchers at Case Western Reserve University have developed a modified radioligand therapy (RLT) for late-stage prostate cancer that is designed to maintain tumor control while reducing damage to the salivary glands, and adverse event that that often leads patients to discontinue their treatments. This approach uses a newly engineered prostate-specific membrane antigen (PSMA)-targeting molecule called PSMA-1-DOTA, which binds more tightly to prostate cancer cells than existing therapeutic ligands and shows significantly lower uptake in salivary tissue.
Details of the development of PSMA-1-DOTA are detailed in a study published in Molecular Imaging and Biology. The new drug has the potential to overcome the barrier to the use of PSMA-targeted radioligand therapy, which is currently restricted to patients who have exhausted all other treatment options because it causes xerostomia—severe dry mouth.
“This breakthrough could fundamentally change prostate cancer care by transforming PSMA-targeted therapy from a ‘last resort’ option to an earlier intervention,” said corresponding author Zhenghong Lee, PhD, a professor in the department of radiology and co-leader of the Cancer Imaging Program at the Case Comprehensive Cancer Center.
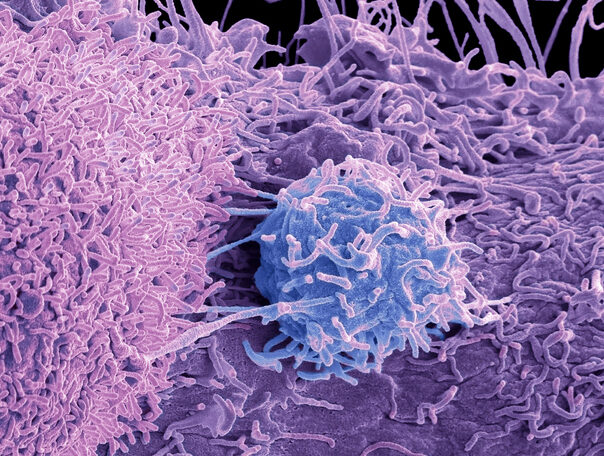
PSMA-targeted radioligand therapy works by attaching radioactive isotopes to small molecules that recognize prostate-specific membrane antigen, a protein that is highly expressed on prostate cancer cells. The radioligands deliver alpha- or beta-particle radiation directly to tumors, to attack tumor cells in patients with end-stage disease. While this approach is effective against cancer cells, PSMA is also taken up by salivary glands, producing radiation injuries that impairs speaking, eating, and swallowing. This “severe salivary gland toxicity, i.e., therapy-induced dry mouth (xerostomia)…has become the dose-limiting toxic side effect for RLT,” the researchers wrote.
The Case Western researchers developed PSMA-1-DOTA via a rational design strategy focused on improving selectivity for tumor tissue. DOTA is a chelating molecule that securely binds radioactive metals, allowing the same targeting compound to be paired with diagnostic or therapeutic isotopes. PSMA-1-DOTA demonstrated four times stronger binding to prostate cancer cells compared to current treatments, a characteristic that shifted uptake of the radioligands away from salivary and lacrimal glands while enhancing delivery to tumors.
Earlier work by the group suggested that a precursor ligand, PSMA-1, when labeled with iodine-125, showed lower salivary gland uptake while still targeting PSMA-expressing tumors. Building on that work, the researchers conjugated PSMA-1 with DOTA to enable positron emission tomography imaging and therapy using clinically relevant radionuclides.
After engineering PSMA-1-DOTA, the investigators compared its effects with concurrently used ligands, including PSMA-11 and PSMA I&T, in mouse models of prostate cancer. MicroPET/CT imaging showed substantially lower uptake of gallium-68–labeled PSMA-1-DOTA in salivary glands and kidneys, while tumor uptake remained sufficient for both imaging and disease treatment. Therapeutic testing with lutetium-177–labeled PSMA-1-DOTA inhibited tumor growth at levels comparable to lutetium-177–PSMA-617, a standard agent.
The researchers also conducted a compassionate-use imaging study in a patient with metastatic castration-resistant prostate cancer at the Technical University of Munich, Germany. Scans of the patient confirmed reduced salivary gland uptake relative to historical data with other PSMA ligands. This “reduced salivary gland uptake…suggests potential for lower normal tissue toxicity in patients when PSMA-1-DOTA is labeled with alpha or beta particle emitting radionuclides, while retaining effective RLT of tumors,” the researchers wrote.
The clinical implications of this newly engineered ligand are significant. Severe xerostomia has limited the both the dose and frequency of PSMA-targeted radioligand therapy, while also typically confining its use to patients with late-stage disease. By reducing salivary gland exposure, PSMA-1-DOTA could broaden the therapeutic landscape to allow earlier use of the therapy.
While promising, the use of PSMA-1-DOTA is still in the proof-of-concept stage. The Case Western team is now preparing for a small clinical trial that will enroll around 12 patients to refine dosing and validate safety. The research will also conducted a preclinical study of PSMA-1-DOTA labeled with actinium-225 to assess salivary gland toxicity in alpha-particle therapy.