Serge Saxonov, PhD, sees biology one cell at a time. Since 2012, he has stood at the center of the single-cell revolution, helping drive a technological leap that fundamentally reshaped how biology is measured. Over the past decade, single-cell RNA sequencing publications have grown exponentially, propelled in large part by Saxonov’s work at 10x Genomics. By commercializing an end-to-end, user-friendly pipeline—from single-cell suspension to confident data interpretation—Saxonov and 10x Genomics eliminated steep technical barriers and democratized access to single-cell biology worldwide.
But behind it all, Saxonov has had a vision that goes beyond the pursuit of academic knowledge—it is to directly improve human health at the point of contact. At the 2026 J.P. Morgan Healthcare Conference, 10x Genomics did its own version of the Neil Armstrong moonwalk, taking its first steps towards clinical integration on biotech’s most scrutinized stage.
“From the very beginning, we have aimed to impact human health,” Saxonov told Inside Precision Medicine. “We started the company with the premise that we wanted to be exceptionally good at building technologies to measure biology. That is our foundational core capability. How we deploy those technologies was always intended to evolve and expand over time.”
The company has announced three major collaborations with leading academic medical centers and plans to establish a CLIA-certified laboratory—signals that its long-standing clinical vision is becoming reality. These partnerships, spanning oncology and autoimmune disease, embed 10x Genomics’ single-cell and spatial platforms into richly phenotyped patient cohorts. Together, they underscore a growing conviction across medicine: the future of diagnosis and therapy selection lies not in bulk averages, but in cells, tissues, and context. The evolution in biological measurements is becoming clinically tangible.
Three collaborations, one biological throughline
Saxonov emphasized that the move toward clinical applications reflects a convergence of factors rather than a sudden pivot. “Our mission is to accelerate the mastery of biology to advance human health,” said Saxonov. “We focus heavily on users and on understanding how to serve them well. That has always been the goal.”
First is technology maturity. Samples can be collected from almost anywhere and analyzed across diverse formats (e.g., including fixed tissue, whole blood, and FFPE), enabling large, logistically complex clinical studies that were previously impractical. “We can now deploy our tools in a more distributed and simplified way,” Saxonov said.
Second is a “secular” shift in medicine itself. In oncology and immunology in particular, the number of available therapies has exploded, while the ability to match patients to the right drug—or combination—has not kept pace. “Determining which therapy will work for which patient remains a major challenge,” Saxonov said. As choices multiply, the cost of guessing grows higher.
Third is a recognition that much of the past decade’s biological discovery, while scientifically rich, was not designed for clinical evidence generation. “The next major step is to run large, tightly controlled studies that correlate clinical outcomes with biological measurements,” Saxonov said. “That is what we are now embarking on.”
Across all three efforts, the unifying aim is to tightly link clinical outcomes with high-resolution measurements of cells and tissues. “The biology that informs therapy selection resides in cells and tissues,” Saxonov said. “That is where disease occurs and where transitions between disease and health take place.”
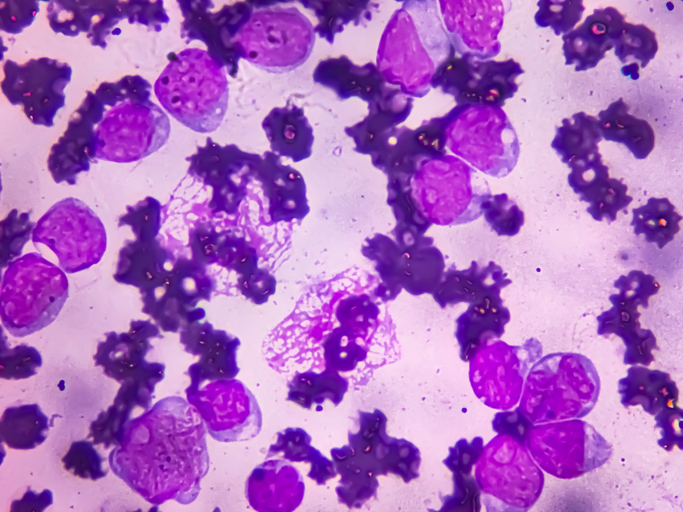
First, 10x Genomics and Dana-Farber Cancer Institute will analyze hundreds of patient tumor samples to pinpoint therapeutic targets and biomarkers, including tumor-microenvironment features tied to treatment response. While genomic profiling reshaped oncology, many patients—especially in immuno-oncology—still move from therapy to therapy without clear guidance. This collaboration aims to change that by translating spatial and single-cell insights—target expression, immune contexture, and signals of drug sensitivity—into actionable clinical reports that help oncologists make smarter, faster decisions.
Second, a partnership with the Cancer Research Institute (CRI) launches an ambitious AI-driven immuno-oncology initiative. By combining 10x Chromium single-cell and Xenium spatial technologies with advanced AI, the team will build one of the world’s largest translational and preclinical immuno-oncology datasets—over 20,000 samples—linking deep biology to outcomes to move from description to prediction.
Third, 10x expands into autoimmune disease with Brigham and Women’s Hospital. Studying 1,000 patients with rheumatoid arthritis, lupus, and giant cell arteritis, the team will use longitudinal single-cell profiling to uncover immune signatures of disease activity, treatment response, and resistance—bringing precision guidance to a field that urgently needs it.
From complexity to clinical action
Perhaps the most defining announcement is 10x Genomics’ plan to establish a CLIA-certified laboratory, which Saxonov said the company intends to set up within about a year. The lab would allow clinicians, initially at academic medical centers, to send patient samples for comprehensive single-cell and spatial analysis as a clinical service.
“This is driven by real demand,” Saxonov said. “Physicians at academic medical centers routinely tell us that it would be transformative if they could send patient samples for this kind of analysis, because such a capability does not currently exist.”
While many companies develop clinical assays, 10x believes its vertically integrated position building the instruments, assays, and analysis pipelines gives it an advantage. “We can build and operate a clinical lab more efficiently and effectively than others because we understand the technologies deeply, can iterate rapidly, and already have the infrastructure, expertise, and partnerships in place,” Saxonov said.
Importantly, the move into diagnostics is not separate from 10x’s research business. Instead, Saxonov framed it as mutually reinforcing. Biopharma companies, Saxonov noted, invest in biomarkers early but need confidence that those biomarkers can eventually be deployed clinically. A clear clinical pathway can de-risk research investment, while clinical adoption, in turn, validates the underlying technologies.
One of the central challenges ahead is translation: turning extraordinarily complex biological data into outputs that are simple, standardized, and actionable for physicians. Saxonov noted that the field’s experience over the past 10 to 15 years in developing NGS-based clinical reports will greatly inform this strategy. “For clinical use, outputs must be synthesized, actionable, and simple,” Saxonov said. “We must work closely with practicing physicians to ensure results are presented in the right format for patient care. There is still work required to converge on standardized data analysis and processing methods that are distinct from research workflows.”
This tension between biological richness and clinical simplicity is not new. Saxonov pointed to the evolution of cancer diagnostics, where early hopes that single-marker PCR tests would suffice gave way to comprehensive genomic profiling as treatment options multiplied. The same logic, Saxonov argued, applies to cellular and spatial biology. “Comprehensive testing is ultimately necessary—history shows this,” said Saxonov. “When mutation-targeted therapies emerged, many believed PCR-based single tests would suffice. In practice, as the number of possible treatments and combinations grew, that approach became impractical. Comprehensive tests are more efficient, clinically useful, and not ultimately more expensive, especially when vertically integrated.”
What excites Saxonov most is the prospect of closing the loop between patient care and technology development with tools like longitudinal single-cell profiling of blood samples. By feeding clinical data back into assay design and analysis, 10x aims to accelerate innovation while building a scalable clinical business.
“There is immense signal in monitoring how a patient responds to therapy changes, particularly through blood-based measurements of the immune system,” said Saxonov. “While circulating tumor DNA has been transformative in oncology, the immune system is uniquely informative because it evolved specifically to detect and respond to disease. Directly measuring it provides a high-fidelity view of what is happening in the body.”
Ultimately, Saxonov framed the company’s expansion as a step toward a long-standing goal rather than a departure from it. “The better we can measure biology with high fidelity,” Saxonov said, “the closer we get to truly personalized treatment for each individual patient.”
CRI’s discovery engine
For the CRI, the partnership with 10x Genomics reflects a broader strategic bet on the future of biomedical discovery—one in which artificial intelligence is only as powerful as the biological data used to train it. CEO Alicia Zhou, PhD, who took on the role a bit over a year ago, told Inside Precision Medicine, “One of the things I felt was really important is that we all recognize that the next generation of biomedical discovery is going to be driven by some version of AI integrated into discovery.”
While advances such as AlphaFold have demonstrated the power of AI in biology, Zhou emphasized that prediction ultimately depends on high-quality, ground-truth data to develop foundation models. “I came in with this thesis at CRI that algorithmic and compute technologies are becoming better, faster, and more automated in their ability to make predictions,” Zhou said. “Ultimately, though, those algorithms need to be trained on ground-truth data that actually tell us about the biology.”
That conviction led CRI to launch the CRI Discovery Engine in partnership with 10x Genomics—a large-scale, open-access effort to generate a high-resolution, single-cell and spatial dataset focused on immunotherapy. Using commonly studied mouse cancer models, the project will systematically perturb tumors with checkpoint inhibitors such as PD-1 and CTLA-4, both alone and in combination, while also examining high-profile failures like TIGIT inhibition.
“The question is whether we could have anticipated that,” Zhou said of past clinical disappointments. “Could we understand the underlying biology well enough to predict when something will work in clinical trials and when it will fail? With higher-resolution data, we may learn that some combinations that failed in clinical trials could have succeeded with different sequencing or timing. That nuance is exactly why this level of resolution is necessary.”
The Discovery Engine will also examine treatment sequencing and timing, tracking biological changes over time and space using single-cell RNA sequencing, spatial transcriptomics, and flow cytometry. “Predicting biology, especially in immunotherapy, is a highly multidimensional problem,” Zhou said. “The administered drug is really a prodrug—the true drug is the immune cell itself. We activate or manipulate immune cells, and those immune cells then become the agents that target cancer. It’s a very complex system, and it’s possible that we’ve accumulated many false negatives over time—mechanisms that are biologically real but failed because they weren’t used in the right combination or at the right time.”
CRI will release the dataset as an open-access resource, positioning it as a foundation for virtual cell models and in silico experimentation. “Bench science often relies on the most convenient model,” said Zhou. “My hope is that instead, researchers will ask whether a model is actually the right one for the question they’re trying to answer.”
For Zhou, the effort reflects CRI’s role not just as a funder, but as a convener of shared scientific infrastructure. “Publicly or nonprofit-funded endeavors are more easily made accessible,” she said. “I felt strongly that this missing piece for accelerating AI-driven discovery needed to be open access, and that CRI should help lead that effort.”
Closing the precision medicine loop
Ultimately, both Saxonov and Zhou see today’s investments as laying the groundwork for a future where biology can be interrogated—and predicted—in silico. “I do think there’s a future where you could run an entirely in silico experiment and say, ‘I’m perturbing this system—tell me what happens,’” Zhou said. “But to get there, you need a massive amount of ground-truth data.”
After a decade of revealing just how complex human biology truly is, the field is now confronting the harder task: translating that complexity into clinical decisions that matter for individual patients. Together, 10x Genomics’ push into diagnostics and partnerships such as the one with CRI open into high-resolution discovery, marking a turning point for precision medicine.
The Discovery Engine and 10x Genomics’ JPM announcements illustrate a new future of precision medicine—and of turning AI from promise into practice in immunotherapy and beyond—that will depend not just on sequencing genes, but on systematically generating high-resolution biological data across cells, tissues, and immune systems, linking it to outcomes, and making it broadly accessible for routine clinical care.
By pairing industrial-scale single-cell and spatial measurement with rigorous clinical studies, standardized workflows, and feedback from real-world care, 10x and its partners are attempting to close a long-standing gap between discovery and application. If successful, this shift could redefine diagnostics—not as blunt, population-level proxies, but as dynamic, cellular readouts of disease—bringing medicine closer to its long-promised goal of truly personalized care.