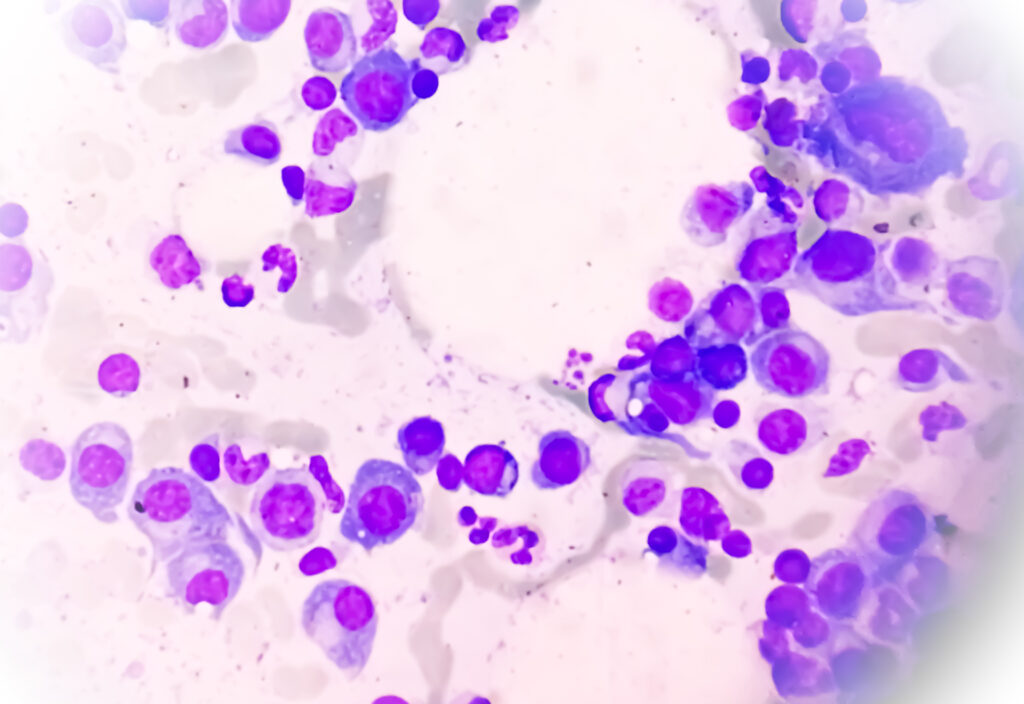
Multiple myeloma, the second most common blood cancer in the United States, is diagnosed about twice as often in men as in women. While this disparity has been recognized for decades, the biological reasons behind it have remained unclear. A new peer-reviewed study published in Cancer now provides one of the most detailed explanations to date, demonstrating that men not only develop multiple myeloma more frequently, but also present with more aggressive disease at diagnosis.
Researchers analyzed data from 850 patients with newly diagnosed multiple myeloma enrolled in the Integrative Molecular And Genetic Epidemiology (IMAGE) study at the University of Alabama at Birmingham. The cohort was deeply characterized, allowing investigators to separate biological sex effects from lifestyle, socioeconomic, and demographic factors.
Men present with more advanced disease
Across the cohort, male patients were significantly more likely to be diagnosed with advanced International Staging System (ISS) stage III disease. They also showed higher myeloma burden, reflected by elevated serum monoclonal protein levels, greater organ damage, and more extensive bone involvement.
Kidney failure, a major driver of morbidity in multiple myeloma, was notably more common among men. Importantly, these differences persisted even after adjusting for age, race, body mass index, smoking status, alcohol use, education, and income. This suggests that delayed diagnosis or healthcare access alone cannot explain the sex gap.
“These findings suggest that sex-specific mechanisms promote multiple myeloma pathogenesis, which may account for the excess risk seen in men,” said lead author Krystle L. Ong, PhD.
Distinct clinical and biological features by sex
Beyond disease stage, the study revealed that myeloma presents differently in men and women at a biological level. Men were more likely to have κ light-chain disease and less likely to have low bone mineral density at diagnosis. Certain myeloma-defining features, such as patterns of organ damage, also differed by sex.
Several of these distinctions were most pronounced in younger patients, suggesting that sex-related biological influences may shape disease initiation and early progression rather than only late-stage outcomes.
Genetic clues point to early disease initiation in men
Genomic analyses offered further insight. Certain chromosomal abnormalities associated with myeloma initiation were observed more frequently in younger male patients. While overall rates of high-risk cytogenetics were not dramatically different between men and women, the timing and combination of these genetic events may contribute to the higher tumor burden seen in men at diagnosis.
These findings support the idea that myeloma may begin earlier or evolve more aggressively in males, long before clinical symptoms emerge.
Implications for precision medicine and early detection
From a precision medicine perspective, the study highlights sex as an underutilized biological variable in multiple myeloma care. Current risk stratification models rely heavily on cytogenetics, tumor burden, and response to therapy—but rarely incorporate sex-specific disease biology.
“These findings may be used to improve risk stratification, diagnosis, and tailored treatments for both men and women with newly diagnosed multiple myeloma or related early precursor conditions,” Ong said in a press release.
In the future, integrating sex-specific risk profiles could improve screening strategies for precursor states such as monoclonal gammopathy of undetermined significance (MGUS), particularly in men who may be predisposed to faster progression.
Toward sex-aware cancer care
While the study does not yet change clinical guidelines, it provides a strong biological foundation for understanding why multiple myeloma disproportionately affects men. By demonstrating that the disparity reflects intrinsic disease biology rather than behavioral factors alone, the work moves the field closer to sex-aware oncology.
As researchers continue to explore how genetics, immune regulation, and hormonal signaling differ between men and women, these insights may ultimately lead to more equitable, earlier, and more effective interventions for multiple myeloma—tailored not only to the tumor, but also to the patient.