Targeting specific mutations during meningioma therapy is feasible and useful, according to a new study. The trial looked at using abemaciclib in patients whose tumors have NF2 or CDK mutations. The study was from The Alliance for Clinical Trials in Oncology and the paper appeared in Nature Medicine.
The Alliance A071401 trial followed patients with grade 2 or 3 meningiomas with those specific mutations. All patients evaluated had previously received surgery, radiation therapy, or both. Patients received an average number of nine cycles of abemaciclib, an oral CDK inhibitor that is currently approved for certain breast cancers.
“The broader goal is to move the field toward precision-based systemic therapies for meningioma, similar to what has happened in other solid tumors,” senior author Priscilla Brastianos, MD, told Inside Precision Medicine. She is a neuro-oncologist with the Mass General Brigham Cancer Institute and co-chair of the Alliance Neuro-Oncology Committee.
The Alliance comprises more than 25,000 cancer specialists at 115 main institutions and 1,400 affiliates across the U.S. and Canada.
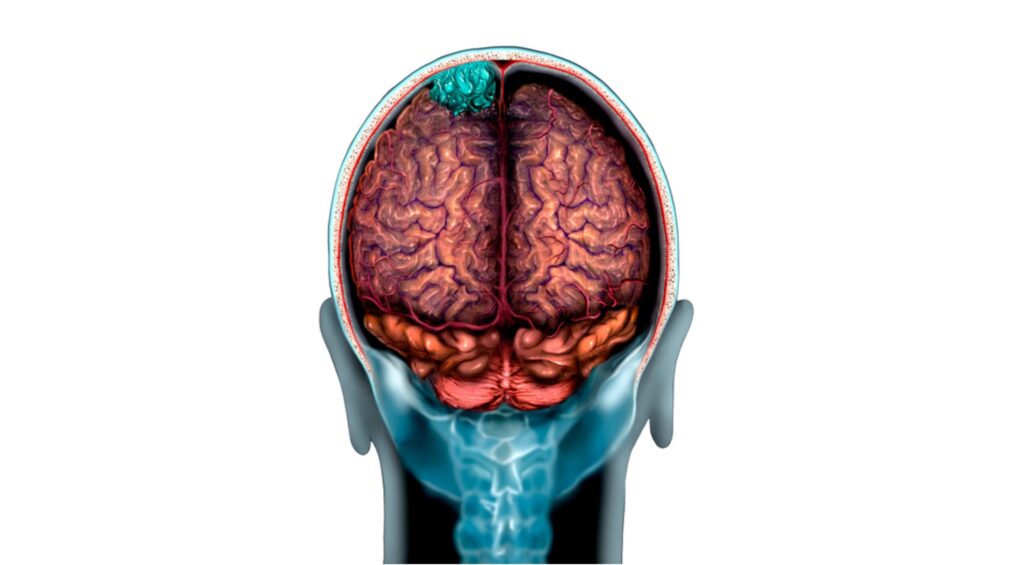
Meningiomas are the most common primary brain tumors. Several systemic therapies have been evaluated in patients with recurrent and progressive meningiomas, with limited success. Research on these tumors has been hampered, the study authors say, by the lack of knowledge of the molecular drivers of meningioma. But, over the last decade, “seminal papers” have characterized the genetic landscape of meningioma and opened up new avenues for the diagnosis, classification, and treatment of meningiomas.
In this study, of the first 24 patients treated with abemaciclib, 58% had high-grade tumors that didn’t progress within the six months after they started therapy. There was no control arm since there are no standard treatment options available for patients with high-grade tumors after surgery and radiation. However, the group’s results compare favorably to previous studies that found that, on average, 0%-29% of patients with grade 2 or 3 meningiomas had cancer that wasn’t progressing within six months from the time they started their experimental treatment.
The median progression-free survival was 10 months, and the median overall survival was 29 months. Side effects were similar to what patients taking CDK inhibitors for other cancers experience. Common side effects included diarrhea, fatigue, headache, and nausea/vomiting. About a quarter of patients had a severe side effect (grade 3 or grade 4) that was possibly or likely related to treatment.
“We chose to study abemaciclib because alterations in the CDK4/6 cell-cycle pathway and loss of NF2 are common drivers of aggressive and recurrent meningiomas,” said Brastianos.
“Preclinical models show that NF2 and CDKN2A/CDKN2B loss leads to unchecked cell-cycle progression, and that CDK4/6 inhibition can slow tumor growth. Abemaciclib is an oral and well tolerated CDK4/6 inhibitor with continuous dosing, making it a strong candidate to test in this setting where systemic options are otherwise very limited.”
She pointed out that since patients with progressive grade 2 or 3 meningiomas who have exhausted surgery and radiation have very limited systemic treatment options, seeing durable disease stabilization and improved progression-free survival with a well-tolerated oral therapy is clinically meaningful. These results, she said, provide a strong biological and clinical rationale to further investigate CDK4/6 inhibition in molecularly selected meningioma populations.
She added that, “Next steps include refining predictive biomarkers, exploring other drug therapies, and designing follow-up studies to better define which patients benefit most.”