Researchers at the University College London (UCL) have identified a central target for immune cells found in the gut in the early development of Parkinson’s disease. Working in mouse models, the team found that muscularis macrophages in the gut engulf misfolded alpha-synuclein, become dysfunctional, and promote immune responses that enable disease pathology to travel along the gut–brain axis. The findings, published in Nature, show that immune cells are active participants in Parkinson’s development and progression, and provide a new therapeutic target that could alter disease development before motor symptoms appear.
“Our study shows that immune cells are not bystanders in Parkinson’s; these gut macrophages are responding, albeit in a dysfunctional way,” said co-lead author Soyon Hong, PhD, group leader at the UK Dementia Research Institute at UCL. “This presents an opportunity to think about how we can boost the function of the immune system and these cells, so that they respond in the correct manner and help to slow or stop the spread of disease.”
Scientists have long suspected that Parkinson’s may begin in the gut and not the brain. One reason is that one of the brain regions affected early in disease onset is the dorsal motor nucleus of the vagus nerve, which directly connects the brainstem to the gut. Clinical observations have also supported this theory, with 50% to 90% of people with Parkinson’s experiencing some form of gastrointestinal symptoms such as chronic constipation decades before developing motor symptoms. Patients with Parkinson’s are delineated as either “body-first” or “brain-first” depending on where the disease first takes root. Body-first Parkinson’s patients account for roughly two-thirds of those who suffer from the disease.
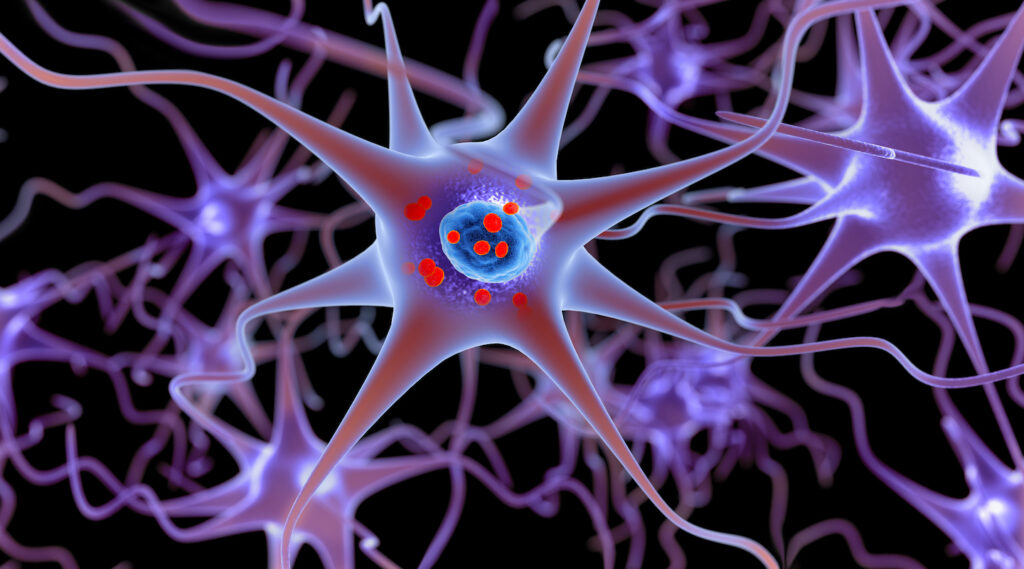
In this new research, the UCL-led team focused on muscularis macrophages (ME-Macs), immune cells that reside in the muscularis externa of the intestine and help maintain enteric nervous system (ENS) integrity. Using mouse models of Parkinson’s, including animals injected with patient-derived alpha-synuclein (αS) isolated from the brains of people who had died with the disease, the researchers tracked how pathology developed after tiny amounts of misfolded alpha-synuclein were introduced into the small intestine.
The data showed that macrophages, rather than enteric neurons, contained most of the misfolded and aggregated alpha-synuclein. These macrophages showed signs of endolysosomal dysfunction, indicating impaired ability to degrade the protein. According to the researchers, “ME-Macs contain misfolded αS, adopt a signature reflecting endolysosomal dysfunction and modulate the expansion of T cells that travel from the ENS to the brain.”
The study also discovered a link between innate and adaptive immunity. After engulfing alpha-synuclein, gut macrophages signaled to T cells, leading to their expansion in the ENS. These “gut-instructed” T cells then migrated to the brain as pathology progressed. Depleting macrophages in the gut of the mouse models or blocking T cells resulted in a reduction of neurodegeneration or motor dysfunction.
“Directed ME-Mac depletion leads to reduced αS pathology in the ENS and central nervous system, prevents T cell expansion and mitigates neurodegeneration and motor dysfunction,” the researchers wrote.
This also helps explain why immune responses may be involved early in Parkinson’s disease development. Previous research has found that circulating T cells reactive to alpha-synuclein are present in patients years before diagnosis.
Co-lead author Tim Bartels, PhD, an associate professor of neurology at UCL said the long time it takes for Parkinson’s develop and progress makes early intervention key to better treatments. “Understanding how Parkinson’s begins in the body could allow us to develop simple blood tests to screen for it, enabling diagnosis long before damage to the brain starts,” he said. “Having the ability to detect and manage Parkinson’s before it even reaches the brain could have a huge impact for those affected.”
Based on these finding, the researchers now plan to find out how immune signaling between the gut and brain could be targeted therapeutically. They also intend to further investigate ways that inflammatory markers in blood could be used for earlier diagnosis. Finally, the team will investigate how macrophage-T cell interactions are regulated and if there is potential to modulate these activities to slow or prevent the spread of alpha-synuclein pathology in Parkinson’s disease.