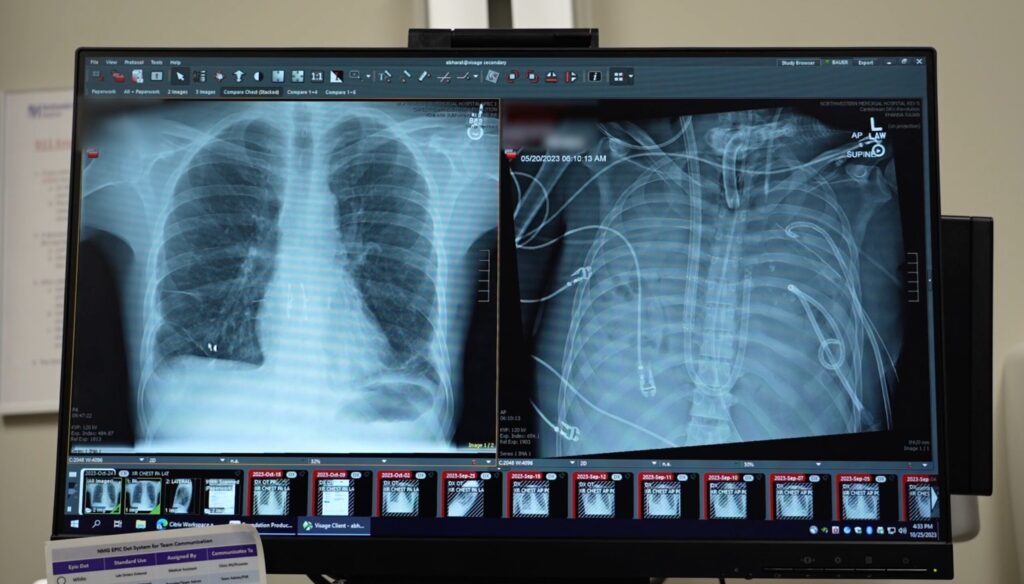
A total artificial lung system kept a patient in critical condition alive for two days without lungs, helping stabilize him enough to receive a life-saving lung transplantation. Two years later, the patient has fully recovered and shows excellent lung function.
A study published today in the Med journal details the procedure, which took place at Northwestern University’s Feinberg School of Medicine. Unlike previous artificial lungs, the system used in this study was designed to adapt to changes in blood flow, significantly reducing the risk of stroke and heart attack associated with the use of existing lung replacement equipment.
The 33-year old patient had developed severe acute respiratory distress syndrome (ARDS) due to an influenza infection, further complicated by a bacterial pneumonia that caused septic shock. The mortality rate for patients with these complications is higher than 80%; However, they are rarely considered for a lung transplant.
“Conventionally, lung transplant is reserved for patients who have chronic conditions like interstitial lung disease or cystic fibrosis,” says Ankit Bharat, MD, thoracic surgeon at Northwestern University and senior author of the study. “Currently, people think if you get severe ARDS, you keep supporting them and ultimately the lungs will get better.”
In this case, the patient’s condition was deteriorating fast and the lungs were damaged beyond repair due to the infections, making a double lung transplant his only option. “He was critically ill. His heart stopped as soon as he arrived,” says Bharat. “When the infection is so severe that the lungs are melting, they’re irrecoverably damaged.”
Bharat and colleagues engineered an artificial lung system that fully replaced lung function by removing carbon dioxide and injecting oxygen into the blood while maintaining a stable flow. This allowed them to surgically remove the infected lungs, which helped stabilize the patient’s blood pressure and keep the infection and bay, allowing his condition to improve enough to receive a transplant. Two days later, donor lungs became available and the transplant was performed.
An analysis of the removed lungs using single-cell and spatial transcriptomics revealed signs of irreversible tissue damage across seven distinct lung regions, featuring molecular signatures of end-stage fibrotic lung disease. These results showed that some patients diagnosed with ARDS may not be able to recover on their own.
“For the first time, biologically, we are giving molecular proof that some patients will need a double lung transplant, otherwise they will not survive,” says Bharat. “In my practice, young patients die almost every week because no one realized that transplantation was an option. For severe lung damage caused by respiratory viruses or infections, even in acute settings, a lung transplant can be lifesaving.”
Conventional histopathology exams are currently insufficient to determine the extent of damage to the lungs caused by ARDS and therefore whether the patient will be able to recover without a transplant. Bharat and colleagues stressed that future studies in larger patient cohorts will be essential to identify biomarkers that can reliably distinguish patients with recoverable injuries from those with irreversible damage, enabling earlier referrals for transplantation for those who need it and thus improving their chance of survival.