Researchers from the University of Michigan researchers have identified the metabolite itaconate as a potential therapeutic target for ZFTA–RELA+ ependymomas, a rare type of pediatric brain tumor. In a study published in Nature, the team showed how tumor cells produce the metabolite itaconate to sustain the cancer-driving fusion protein ZFTA–RELA that helps promote tumor growth.
“We were surprised that a brain tumor produces a metabolite that is usually made by immune cells,” said first author Siva Kumar Natarajan, PhD, a postdoctoral research fellow in the Venneti lab at the University of Michigan. “We wanted to find out what itaconate was doing in these tumors.”
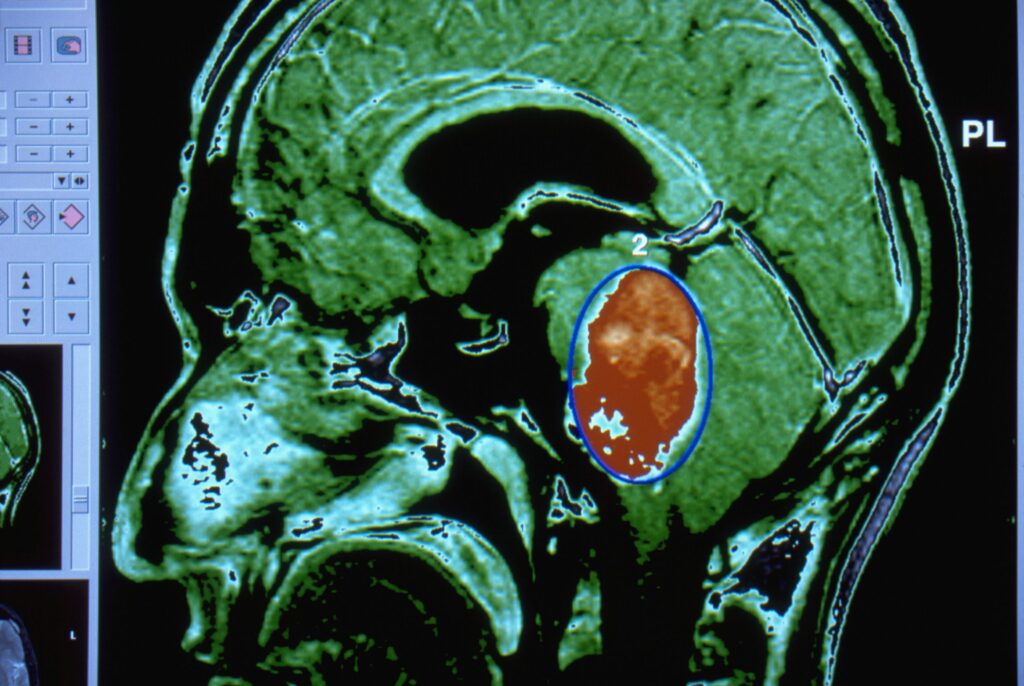
Ependymomas are tumors that arise in the brain or spinal cord and are the third-most common type of brain tumor in children. They affect about 250 children in the United States each year and are most often diagnosed in children eight years and younger. The main forms of treatment for these tumors include surgically removing the tumor followed by radiation and chemotherapy, though chemotherapy hasn’t been shown to be consistently effective. Currently, there are no targeted therapies or clinical trials targeting ZFTA-driven ependymomas.
The researchers noted that neither ZFTA nor RELA alone is oncogenic, but together the ZFTA–RELA fusion have been shown to be a potent oncogene that can transform cells in vitro and in vivo. For this current study, the Michigan team began with understanding that metabolic reprogramming is a common feature of cancer development and that certain metabolites drive tumorigenesis by altering epigenetic regulation. To explore whether ZFTA–RELA reshapes metabolic–epigenetic pathways, the researchers analyzed human ependymoma tumor samples, patient-derived cells, and animal models. Using cell lines from mice and patients as well as in vivo models, they identified production of itaconate within ZFTA–RELA+ tumor cells.
Mechanistically, the investigators found that itaconate epigenetically activates ZFTA–RELA transcription by enriching activating H3K4me3 marks through inhibition of the H3K4 demethylase KDM5. The tumors also enhanced glutamine metabolism to supply carbon for itaconate synthesis. Importantly, the investigators found that in mouse models of the tumors, preventing ACOD1 from producing itaconate reduced tumor growth. Inhibiting the feedback loop lowered ZFTA–RELA levels and led to tumor shrinkage.
“Our findings also have translational relevance, as inhibition of PI3K signaling and glutamine metabolism led to therapeutic effects in multiple ZFTA fusion models,” the researchers wrote.
The U of M team noted that earlier research had established that ZFTA–RELA is sufficient to drive tumor formation but had not found ways that it could be addressed to reduce its promotion of tumor growth.
“This is the first study to show that the ZFTA-RELA fusion can be targeted in this type of tumor,” said senior author Sriram Venneti, MD, PhD, a professor of pathology and pediatrics at U of M and a member of the Rogel Cancer Center. “We are hoping to expand this study to protein fusions that function similarly in other types of cancer.”
Building on these findings, the researchers are now working with the Pediatric Neuro-Oncology Consortium to develop a clinical trial targeting the itaconate pathway in patients with ependymomas.