Evelyne Bischof on why credible training of doctors in healthy longevity is one of the most important health innovations of our time.
Longevity Education Hub has published the first original research paper demonstrating data on the impact of healthy longevity medicine education for physicians on their actual clinical practice.
Healthy longevity medicine has been a subject of discussion for years. We talked about biomarkers, biological age, prevention frameworks, and systems thinking. The field has examined biomarkers of aging, biological age estimation, preventive care frameworks, and systems-level approaches to health optimization. Researchers and physicians have convened at numerous scientific conferences to refine concepts and advance translational implementation. Yet, much of this discourse has remained conceptually rich but operationally underexamined, with limited empirical insight into how these ideas translate into routine clinical care.
One practical question has quietly lingered in the background: what actually happens when you teach longevity medicine to practicing physicians? The Longevity Education Hub recently published an international research study offering the first empirical data showing whether structured education changes real-world medical practice.
While HLM was shaping up in early 2020, with the first publication mentioning the name ‘longevity medicine’ , there was a big gap between demand and science versus delivery of the science to patients in the clinic. This is where the Longevity Education Hub was born. Established as a global, volunteer-driven initiative, the Hub set out with a mission to provide credible, evidence-based education in healthy longevity medicine that is accessible to physicians everywhere, entirely free of charge, while translating the latest expert-aligned advances in geroscience into clinically actionable knowledge suitable for everyday medical practice
Since its launch, the Longevity Education Hub has reached an important milestone. Implementation at NHS HDRUK, followed by establishing eight national chapters, and most importantly its structured curriculum has now been implemented into the formal medical curriculum in four medical schools, helping integrate longevity science into mainstream medical education rather than leaving it as an optional benefit. Since its establishment, the Hub has taught over 12,000 physicians worldwide. These are general practitioners, internists, specialists, and healthcare professionals from dozens of countries who have sought a deeper understanding of how aging biology can inform preventive care.
But enthusiasm alone is not enough. If healthy longevity medicine is to become a credible part of clinical practice, it must be evaluated, measured, and studied just like any other medical discipline.
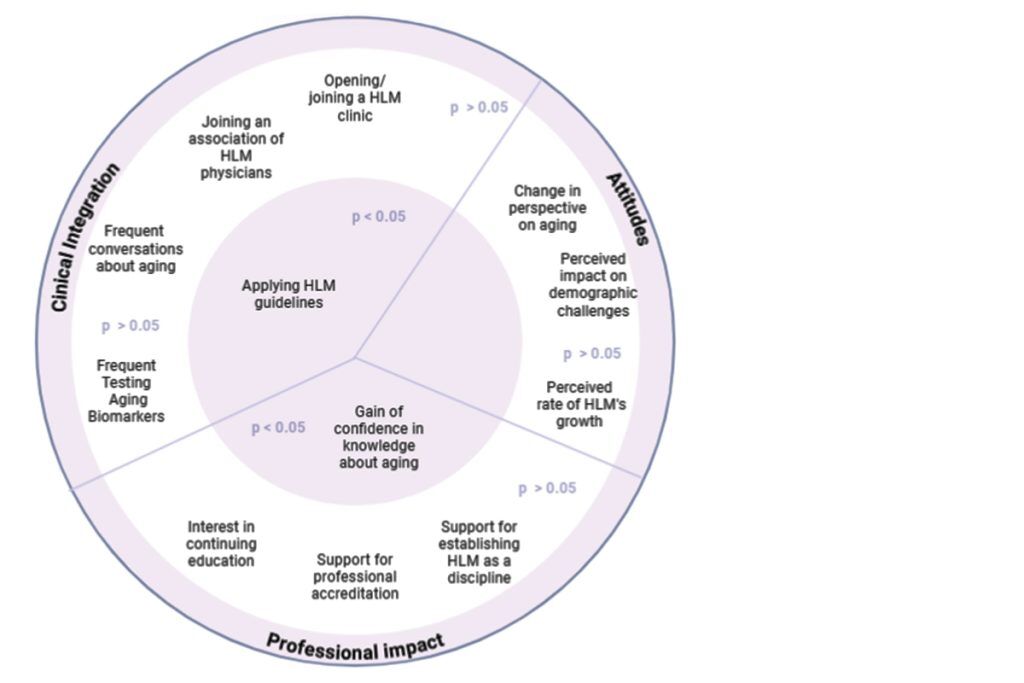
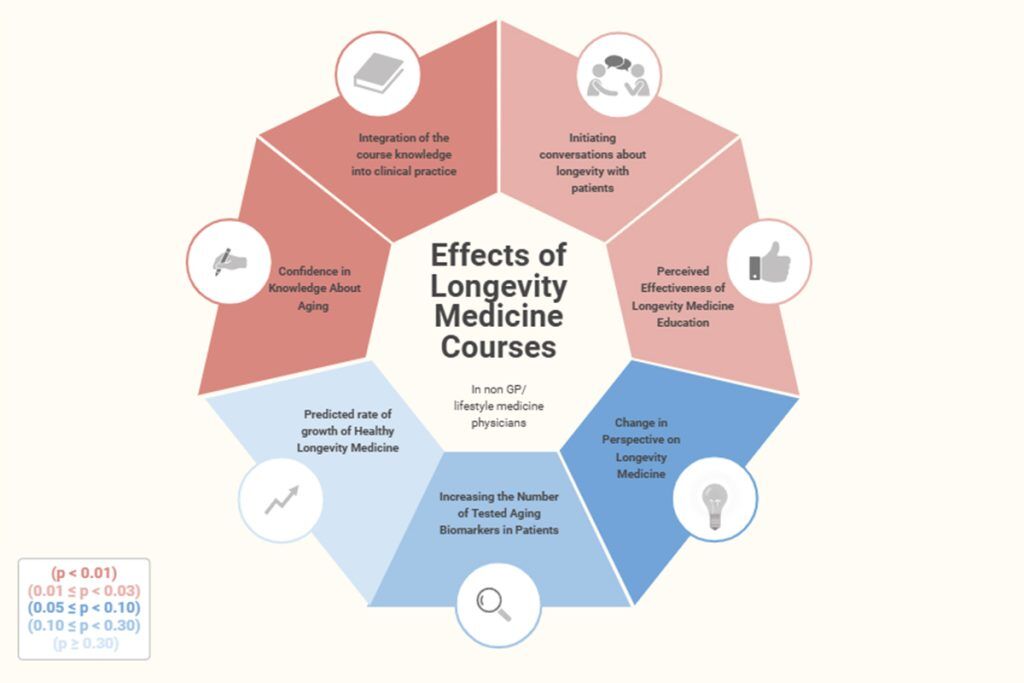
That is why a recently published peer-reviewed study in JMIR Medical Education is so significant. For the first time, researchers systematically examined the impact of a structured healthy longevity curriculum on practicing physicians across 42 countries. The study assessed whether education translated into measurable shifts in confidence, perspective, and clinical behavior. It evaluated a structured Healthy Longevity Medicine curriculum delivered to physicians across multiple regions. The goal was modest and practical: assess whether the course influenced how doctors approach patients, discuss prevention, and interpret emerging longevity tools.
Physicians reported that the education helped them feel more comfortable initiating conversations about healthspan and prevention. Many shared that they previously avoided the topic because it felt either too abstract or too vulnerable to hype. After completing the curriculum, they described feeling better equipped to stay within evidence-based boundaries while still engaging patients’ curiosity.
In other words, education created confidence.
Why does it matter? Without structured and credible education, the field risks being overtaken by misinformation. The word “longevity” is increasingly associated with expensive, unproven interventions. That trajectory is neither equitable nor sustainable.
The message of this study is clear: when doctors are given rigorous, evidence-based training in healthy longevity medicine, they respond positively and apply it responsibly. Education becomes the bridge between scientific discovery and patient care.
Dr Alex Zhavoronkov, senior author of the paper and founder of the Hub, said: “The progress in longevity biotechnology and in AI is accelerating. In addition to measuring aging utilizing traditional aging clocks and foundation models, we see the first potential longevity therapeutics in clinical trials. It is very important to up skill physicians to facilitate biomarker-augmented clinical trials and to prepare for deployment of longevity medicine in the clinic.”
Dominika Wilczok, Duke student and coordinator of LEH, added: “The great virtue of Longevity Education hubs is the accessibility. The Longevity Education Hub operates through the voluntary efforts of clinicians, scientists, and educators who believe that foundational knowledge about aging biology should not be hidden behind paywalls or limited to elite institutions.”
The global participation in the curriculum demonstrates a strong appetite among physicians for structured, scientifically grounded training in this area. The long-term vision is not to create a niche specialty. It is to integrate healthy longevity principles into everyday primary care – where the majority of health decisions are made. A shift from reactive medicine to proactive, resilience-focused care requires not only innovation in laboratories, but transformation in classrooms and clinics.
What makes this initiative particularly meaningful is that the curriculum is no longer confined to workshops or private courses. Healthy longevity medicine is gradually entering universities – not as an alternative to traditional medicine, but as an extension of preventive, evidence-based care. It has already been implemented in formal academic settings in six countries.
Importantly, this entire effort has been built by volunteers – physicians and scientists at different stages of their careers – all working to translate longevity science responsibly into practice. Contributors from multiple countries have helped develop modules, review materials, share cases, and refine standards. The publication acknowledges them individually because this is very much a collective endeavor.
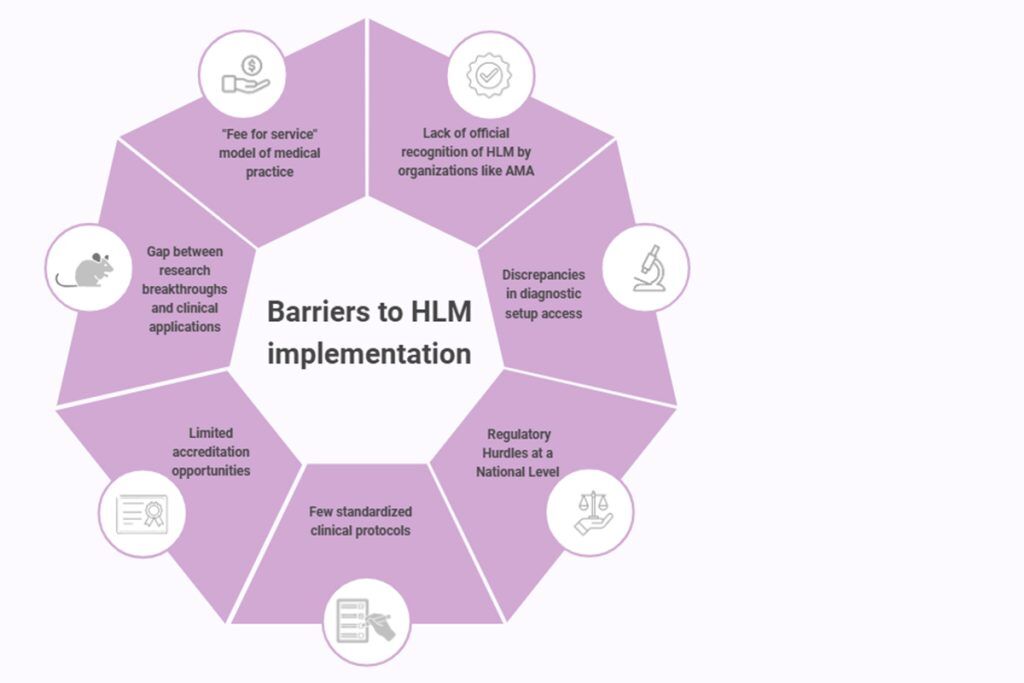
Of course, education alone does not solve everything.
As identified in the discussed publication, physicians still face:
- Limited consultation time
- Reimbursement systems that prioritize treatment over prevention
- Variability in evidence quality across longevity-related tools
- Lack of formal board recognition for the field
These structural challenges are real. They require policy engagement and healthcare system reform.
If there is one takeaway from the study, it is this:
Structured longevity education appears to help physicians feel more grounded. It encourages scientific discipline in a rapidly evolving space. It strengthens patient communication. And it supports a gradual cultural shift toward earlier, anticipatory care based on data.
The work is still young. The field is still maturing. There is much to refine and standardize.
But for perhaps the first time, we can say that longevity medicine is not only being discussed but taught, implemented, and integrated into everyday clinical practice.
In an era of rapid medical change, and sometimes confusion, the foundation must remain solid: credible science, transparent evaluation, and accessible education. Healthy longevity medicine will only become a meaningful, equitable force in global health if it is taught responsibly and shared widely.
Education is not the most glamorous part of medical innovation. But it may be the most powerful.
About Evelyne Bischof

Professor Evelyne Yehudit Bischof, MD, PhD, MPH, FEFIM, is first author of the new paper and co-founder of Longevity Education Hub.
She is a professor at Shanghai University of Medicine and Health Sciences, a visiting professor at Tel Aviv University School of Medicine, Chief Physician of Internal Medicine at University Hospital of Jiaotong School of Medicine Renji, Shanghai and affiliated with the International Center for Multimorbidity and Complexity in Medicine (ICMC), Universität Zürich in Switzerland.
With a research focus on oncology and longevity medicine, AI and digital health, precision medicine, biogerontology and geronto-oncology, Evelyne has published more than 80 peer-reviewed papers; she is frequent speaker at scientific and medical conferences in Asia and Europe and a long term member of various medical societies including the European Federation of Internal Medicine, World Academy of Medical Sciences and the Swiss Society of Internal Medicine. Evelyne also sits on several scientific and advisory boards of biotech and longevity hubs.

