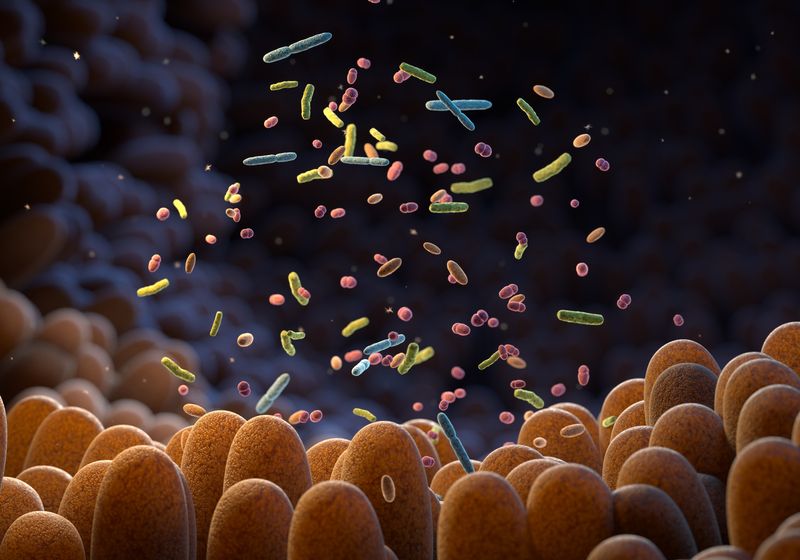
Over the past few decades, researchers studying the gut microbiome have noted associations between gut microbes and neurological conditions from depression and Parkinson’s disease to autism spectrum disorders.1 With bidirectional communication between the gut and the brain via the vagus nerve, the potential role of the gut microbiome in autism spurred numerous investigations from human observational and mechanistic mouse studies to interventional clinical trials.
However, in a Perspective paper published today in Neuron, scientists argue that research on the connection between the gut microbiome and autism has methodological, conceptual, and statistical flaws.2 The authors of the article, led by Kevin Mitchell, a developmental neurobiologist at Trinity College Dublin, dug into the autism-gut microbiome literature and concluded that there is no evidence that the gut microbiome causes autism. Researchers who study the connection between the gut microbiome and autism, however, take issue with the authors’ characterization of their work. The autism-gut microbiome researchers argue that they are not saying that gut microbes cause autism but that there is an association between the two that may be targetable with therapeutics, helping ameliorate some aspects of condition.
“This is kind of a new advent with neuroscience and being able to access the possibility of gut-brain interactions, and I think it’s a really promising field. So, I’m not surprised that the authors are really interested in that,” said Shelly Buffington, a neuroscientist studying the maternal gut microbiome at Baylor College of Medicine. “Overall, however, there’s a basic misunderstanding of the fundamental questions in the field that are being asked and really a mischaracterization of the interpretation of the results that is pervasive throughout the piece.”
Statistical Problems in Genetics Inspired a Closer Look at Autism-Gut Microbiome Research
In his neurobiology research, Mitchell is interested in understanding the origins of neurodevelopmental disorders, including autism. “I mainly work on genetic factors, but [I am] very open to the idea that there could be environmental factors,” he said. As he looked at the studies coming out about the gut microbiome and autism, he felt, for example, that the numbers of subjects or animals included in the research were too low to draw significant conclusions.
He likened this aspect of gut microbiome research to issues in candidate gene association studies that occurred in the past. He explained how researchers might take two populations—for example, people with autism and those without—and look for differences in frequencies of genetic variants.
“Turns out, if you do that in small numbers of people with large numbers of variables to look at, then you’re going to see something that looks like a signal, especially if you don’t have a replication sample, if you don’t correct your stats properly for having done so many tests,” he said. He added that similar issues plagued neuroimaging studies. For example, in analyzing brain scans from people with autism and those without, there are lots of variables to look at and flexibility in how to analyze the data. If scientists use inappropriate statistical tests, this can lead to incorrect conclusions.
“What I was seeing in the microbiome papers was the same kind of design flaws, basically. And so, that prompted us to think maybe we should do a deeper dive on this thing to see if our impression is actually correct.”
When Mitchell and his team assessed the observational studies that analyzed the differences in gut microbiome composition between people with and without autism, they found that the studies had smaller sample sizes than they would need to show an association. Larger studies, they said, seemed to show low associations between the gut microbiome and autism, casting doubt on the link.
What Does Autism Look Like in a Mouse?
Researchers cannot investigate the mechanisms of how the gut microbiome might affect autism in humans, but they can carry out such studies in mice. Mitchell and his colleagues, however, doubted how the seemingly human-specific features of autism could be modeled in a mouse.
“How much a mouse sniffs around at another mouse is a long way away from what we typify in autism as say, not being very well attuned to someone’s body language or not being able to get sarcasm. I mean, these are just so miles apart,” he said.
However, researchers who use these models to study autism don’t claim that the mice exhibit the same exact autistic behaviors seen in humans. In a 2021 interview for a Drug Discovery News story on the gut microbiome and autism, Sarkis Mazmanian, a gut microbiome researcher at the California Institute of Technology, explained, “There’s no such thing as a mouse model of autism. We can model behaviors in mice that are correlates of behavior of humans.”
For example, two mouse models that exhibit some behaviors that are also seen in humans with autism are the Maternal Immune Activation (MIA) mouse model and the maternal high-fat diet model. In the MIA model, pregnant mice are given the flu at a specific gestational age, which results in their offspring exhibiting autism-like behaviors, including impaired social behaviors and communication as well as repetitive behaviors. In the maternal high-fat diet model, the offspring of mothers who ate a high-fat diet display impaired social behaviors.
Of these mouse models, Mitchell said, “The epidemiological links in humans are really shaky.” He added, “There are, again, sort of tiny statistical effects. They tend to disappear in larger samples, but they also disappear if you’re correcting for confounds in the typical way. So, there doesn’t seem to be good evidence that the models that those studies were using have anything to do with autism in the first place.”
The MIA mouse model, however, does lead to neurological changes in the offspring that are often seen in children with autism.3 In terms of the maternal high-fat diet model, Buffington disagreed with Mitchell’s characterization of the model. “I just think that that’s kind of old information. It’s not consistent with what I understand of the literature,” she said. She pointed to data from a large longitudinal study published this year in Nature Metabolism that identified a significant association between high BMI, high risk genetics, and autism.4 She also referenced a study in JAMA Network Open that assessed 85,648 mother-infant dyads in one cohort and 11,670 mother-infant dyads in an independent cohort.5 The authors of that study found that for mothers who had medium-to-high adherence to a healthy diet, their children had a lower risk of being diagnosed with autism. “With low adherence to a healthy dietary pattern, there’s a specific negative impact on social scores,” Buffington said. “Using the microbiome as a therapeutic target to improve outcomes in kids is really viable in my opinion.”
Autism and the Gut Microbiome in Clinical Trials
Another critique Mitchell and his colleagues had was that they did not see that discoveries made in mice were being followed up on in clinical trials, which they took as evidence of the field not progressing. When they found examples of clinical trials that had been done, Mitchell said, “the design flaws are just really obvious.” He added, “If you’re doing small trials like that—open label, no control arm—you’re likely to see things that aren’t real.” Buffington disagreed; there were both examples of clinical trials that followed up mouse studies as well as randomized, blinded, and placebo-controlled trials.
In a 2016 mouse study, Buffington and her colleagues discovered that treatment with a Lactobacillus reuteri strain improved social behaviors in offspring of a maternal high-fat diet mouse model.6 An independent research group then followed up on this study in a randomized, double-blind placebo-controlled trial. In the trial, researchers found that children with autism treated with the same L. reuteri strain showed improved social behaviors on standard autism screening tests.7 They published the results in Cell Host & Microbe in 2024.
“That’s a really great demonstration of mechanistic validity, and that proving out both in these mouse models and then to see it in humans. And this is all within 10 years of each other from one publication to the next,” said Buffington.
Of the small open label trials that have been conducted, some didn’t just measure behavior, but blood metabolite levels too. Mitchell and his colleagues mentioned the initial publication about a trial conducted by Rosa Krajmalnik-Brown, a microbiome researcher at Arizona State University, where she and her team transferred gut microbes from healthy donors to children with autism.8 The researchers found that the children’s behavioral symptoms improved even two years after the end of the treatment period. In a follow up paper analyzing the metabolites in the children’s blood, the researchers found that their blood metabolite composition had become more similar to that of the typically developing children.9
While Krajmalnik-Brown agreed that the behavioral results could have been subject to the placebo effect, she added that when “measuring the metabolites, that’s a lab measurement. There’s no placebo effect. That’s another thing that was minimized in this paper.”
Finally, Mitchell and his colleagues wondered why there were not larger clinical trials being done in the autism-gut microbiome space. According to Krajmalnik-Brown, these trials are underway. “We also have done blinded studies, Phase 2 trials. We haven’t published that, but we actually have done one trial for adults, one for kids, and we’re running a second one for kids,” she said. “What we said was a weakness, we’re actually working now on doing things better. That’s how science advances, and we’re doing research that is both fundamental and applied.”
How Does the Autism-Gut Microbiome Field Move Forward?
In their Perspective piece, Mitchell and his colleagues presented two paths forward for research on the link between autism and the gut microbiome: Perform research more rigorously or stop altogether.
Buffington agreed that more rigorous research is a good thing. “I’m all in on that,” she said. “That’s not unique to the microbiome. I think we should always be striving for increased rigor.”
She added that there are still many important questions on the connection between autism and the gut microbiome that remain unanswered. “It’s not time to give up on this line of investigation by any means,” she said. For instance, when it comes to treating different aspects of autism, the gut microbiome is much more tractable than human genetics.
“We’re not going to be able to use antisense oligos to fix everybody in in utero development that might have some germline mutation or something sporadic, but that doesn’t mean we can’t use targeted intervention to improve [gastrointestinal] distress that then relieves some stress on a child, and it improves their overall behavioral umbrella,” Buffington said.
Krajmalnik-Brown hopes to find biomarkers to help identify people who would most benefit from a treatment targeted to the gut microbiome. “There’s a lot of work that still needs to be done,” she said, “but we can’t do that if we don’t have funding to do it.” She added that she was disappointed to see researchers outside of the field conclude that research on autism and the gut microbiome should no longer be funded.
Buffington explained, “[The gut microbiome is] this big chemical factory inside of us, and we can modify it by pushing this way or that way. But the most important thing is first to know what have we got going on? What’s the functional composition?” She added, “The question that’s dominating the field is not a causality question. It’s really, what’s the relationship here. Is this something that can be a modifier for risk? Is it something that we can actually use as a therapeutic target and deliver for these patients?”