“I’ve fallen and I can’t get up.”
We’ve all seen the infomercial: an elderly person, alone, fallen, unable to reach a phone—an image turned into a selling point for a pendant-style SOS device. But for millions of people living with osteoporosis or age-related loss of bone mineral density (BMD), that dramatized moment is uncomfortably real.
Ben Swanson, DDS, PhD, imagines a future where that device isn’t needed at all—not because help arrives faster, but because people stay on their feet, aging without the burden of fragile, fracture-prone bones. That vision is what drove him to found Skeletalis, a biotechnology startup now emerging from stealth with an $8 million seed round to advance a targeted small-molecule delivery platform for bone disease. The financing will also propel its first candidate, a bone-targeted osteoporosis therapy designed to prevent fractures, maintain BMD, and avoid the safety tradeoffs that have limited existing options.
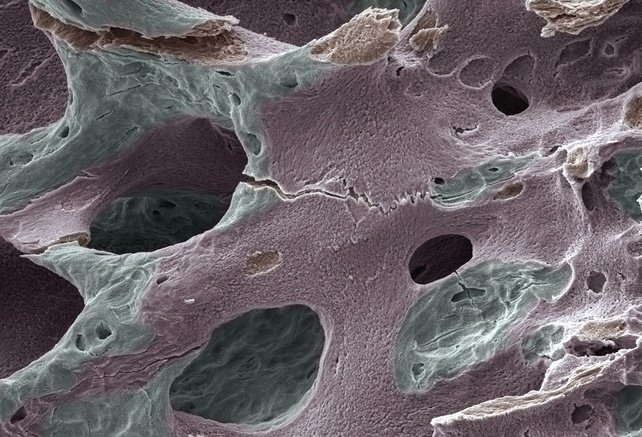
At the center of Skeletalis is the Osteoclast-Activated Skeletal Intervention System (OASIS), a platform built to concentrate therapy precisely where bone loss is occurring—without disrupting the body’s natural remodeling cycles. The premise is deceptively simple: send drugs to the places where bone is actively being broken down and leave the rest of the skeleton alone.
A dentist in drug development
Swanson’s path to biotech leadership is an unusual one. He isn’t a physician or traditional drug developer; he’s a dentist. But his scientific expertise sits squarely at the intersection of bone biology and drug delivery. Over years of clinical practice, as he treated patients experiencing significant bone loss, a recurring pattern sharpened into a motivation.
“Initially, a lot of my work was focused on classical regenerative medicine and tissue engineering, thinking about how we regenerate tissues in a small, very localized compartment,” Swanson said. “The reality that I saw clinically in my patients was that the most pressing need in bone diseases was not necessarily these small, perfectly shaped defects. You could patch something in there, but where the entire skeleton is affected is probably the worst thing that could happen to them in terms of loss of independence. It was really tied to the downfall for a lot of patients who never, ever return home afterwards.”
Dentistry, he says, gave him a front-row seat to patients’ lived experiences with bone-health drugs.
“As a dentist, you get to talk to people when they’re super vulnerable and uncomfortable,” he said, “and started having these conversations with patients and learned very quickly from them about these very personal experiences of the existing drugs that they were taking, yet their bones were getting weaker very quickly. That’s what led me to start thinking critically about how we develop solutions here and really overcome these barriers of the safety concerns.”
The bone-disease field, meanwhile, has stagnated. Over the past decade, it has not enjoyed the kind of national-scale scientific initiatives that buoyed neuroscience, oncology, or even metabolic disease. Several promising drugs failed for safety or efficacy reasons, prompting major pharmaceutical companies to exit the space entirely.
“That got us thinking about what it would take to really unlock the next generation of therapies that would enable disease-specific modulation and really that enhanced safety profile and efficacy that is commensurate to treating a chronic disease,” Swanson said.
Cracking bone diagnostics
The scientific and clinical bottlenecks in musculoskeletal medicine are well known. Proving that a drug prevents fractures—an event that is unpredictable, sporadic, and often geographically separated from clinical sites—makes osteoporosis trials massive, slow, and expensive. Enrollment typically focuses on patients at high fracture risk, further constraining timelines.
“You effectively dose patients and wait for them to fall,” Swanson explained. “Keeping track of that isn’t straightforward because maybe you’re going to fall when you’re on vacation or you’re visiting your family for the holidays. To power these studies, those trials are generally incredibly large. The largest one was about 17,000 patients in a Phase III, which is just prohibitive to do.”
A turning point came through SABRE, an initiative led by the Foundation for the National Institutes of Health (FNIH). In 2013, its Bone Quality Project—now SABRE—began systematically evaluating whether bone mineral density could serve as a surrogate endpoint for osteoporosis drug approvals.
“One of the things about osteoporosis that makes it a little bit unique is that it doesn’t hurt—you’re not in any pain,” Swanson said. “Of course, after a fracture, you’re in pain. So, when we talk about how we intervene and really maximize the opportunity here, it comes down to public awareness and early detection.”
DEXA (Dual-Energy X-ray Absorptiometry) scanners ultimately became the anchor for SABRE’s surrogate-endpoint model. Increasing availability, driven in part by awareness gaps and the obesity epidemic, made DEXA a more routine clinical measurement. The project identified a surrogate threshold effect: a change in BMD that correlates reliably with fracture-risk reduction.
DEXA scanning—cheaper, more common, and more widely understood—is helping clinicians detect disease earlier. “DEXA is an incredibly valuable tool for us,” he said. “More and more people are getting the scans, the data is accessible, it’s routine, and pretty easy… But of course, we’re actively watching for new diagnostics and new tools that can be considered either companions or more tools in our kit to understand the progression and rate of progression of these diseases. But there are clear blood biomarker signatures that we also use to understand the disease.”
Swanson said this shift fundamentally changes what trials can look like. “Whereas with BMD, it’s a defined endpoint. You can define the time period. It’s similar to any other imaging endpoint,” he said. “I think it really opens up a lot of opportunity to do this in an efficient and, again, more faithful way to the disease. That makes it a far more objective, standardized approach than how many stairs do they follow to the ground component? The variables are very much reduced when doing good imaging, like DEXA scanning and marrow density.”
He added, “It’s an exciting resurgence that we’re at the forefront of to capitalize on this shift, and it really represents two things. It’s, of course, easier to do trials now. It’s going to be more efficient, with more sites. You can include a more diverse and broad range of patients. But as a clinician, I can’t help but be excited by this idea that we can now measure the progression of disease rather than just the failure of treatment.”
Skeleton as a substrate
Unlike a knee replacement or a spinal fusion—highly localized interventions—treating osteoporosis means treating all 206 bones. That, Swanson said, requires rethinking delivery from the ground up.
“What we can do is leverage the skeleton effectively like a biomaterial or a substrate that we can drug and coat the entire thing with our molecule,” he explained. “That enables us to intervene much more specifically and then at the same time, minimize systemic exposure. So we’re minimizing the likelihood of off-site and off-target effects by specifically targeting both.”
Bone’s extensive vascular network provides an entry point; OASIS builds on that biology. Systemically administered small molecules typically have poor bone localization, with only a small fraction reaching the surfaces where osteoclasts break down mineralized tissue. The OASIS approach uses blood flow as a “highway,” then employs surface affinity to keep the drug in place.
“When thinking about developing drugs to target and treat bone, very small portions of the drug that are systemic actually get to the bone surface where the disease happens,” said Swanson. “Blood flow is our mechanism, the highway that we use to get to the bone surface, and then the drug is localized by affinity to the surface.”
Skeletalis’ lead molecule stems directly from Swanson’s doctoral work at the University of Michigan, which the company has licensed. The team is now advancing robust preclinical programs, including larger-animal models. “We have some really exciting rodent data that gave us a tremendous amount of confidence in proving the mechanism of an integral part of systemic health, particularly as we get older,” Swanson said.
The big target: postmenopausal osteoporosis
Osteoporosis is far from rare: postmenopausal or estrogen-deficiency osteoporosis represents a little over 70% of all cases. The clinical and public-health burden is enormous—and gendered. Swanson noted that the disease begins before menopause, accelerates after, and continues for decades.
One fracture can significantly worsen outcomes, raising risks for Alzheimer’s disease, dementia, and cardiovascular decline. “One of the things that’s most exciting in this field is that our animal models are very translational,” Swanson said. “There’s also estrogen deficiency-induced disease in rodents and animals, and we also do DEXA scans in these animals. And so it really allows us this swift translational opportunity to validate the technology and really demonstrate for patients what is an efficient and safe development path.”
That doesn’t mean estrogen replacement therapy is the solution, he clarified. “Estrogen replacement therapy is really a totally separate discussion,” Swanson said. “There has been demonstrated efficacy … but I wouldn’t say that it’s generally accepted. Certainly, menopause is one piece of the puzzle here. But what’s interesting is the bone disease actually starts before menopause and continues long after the onset of menopause.”
Swanson’s focus, and the company’s, is targeting the disease process locally and chronically. “Our immediate focus is on osteoprocess and really the idea of localizing both to the tissue and to the disease process, really localizing that therapeutic effect,” Swanson said. “When we think about chronic disease, the goal or the moonshot, is what’s a drug that’s safe and effective to take for the rest of your life?”
He calls this the core vision for Skeletalis. “This is not a disease that goes away, but one that certainly we can manage and prevent the progression of,” he said. “If we can prevent that first fracture from ever happening, we’ve really solved a major public health problem.”
The need extends beyond older women. Patients with cancer, including breast cancer survivors placed in chemically induced estrogen deficiency, face early-life bone-health challenges. “Menopause and estrogen deficiency can happen for a number of reasons throughout someone’s life,” he said. “Patients much earlier in their life, who may be breast cancer survivors, are effectively forced into estrogen deficiency as a way to prevent that disease recurrence. Yet now we have to manage their bone health and other aspects of their health as a result from that.”
A reawakening for bone therapeutics
In a field long overshadowed by bigger, flashier therapeutic areas, Skeletalis hopes to rekindle momentum. The SABRE decision opens regulatory pathways that once seemed closed. Growing public awareness of menopause and midlife health is changing both patient engagement and investment landscapes.
And Swanson believes targeted small molecules—more precise, more durable, and safer—are poised to reshape how the world thinks about bones. In that future, fewer patients will experience the sudden, catastrophic loss of independence that follows a fracture. And far fewer will ever need to reach for an SOS pendant.