Researchers at the University of Michigan have incorporated an RNA-based fusion assay into their standard next-generation sequencing (NGS) panel for acute myeloid leukemia (AML), in order to detect gene rearrangements that cytogenetics often miss. The added element is a probe-ligation–based targeted gene fusion assay that is designed to identify 112 gene fusions that are known to be associated with leukemia.
“We wanted to have the ability to detect gene fusion, especially since now we know that a decent proportion of them are cryptic and missed by routine cytogenetic practice,” said lead author Corey Post, MD, a molecular genetic pathology fellow at Michigan Medicine during a poster presentation last week at AMP.
The assay uses approximately 250 probes against five-prime and three-prime gene partners. For the test, mRNA is extracted, and if a fusion is present, “the five prime and three prime probe will be kneeling adjacent to each other,” Post explained. “Those two probes can then be ligated, and after ligation, amplified, [producing] an amplicon which goes into the sequencing reaction with the patient’s DNA sample.”
The result is a single test for both sequencing and fusion detection. The major advantage of this method is that there is only an amplicon if a fusion is present, so there is no impact from this to the sequencing depth of other targets if the sample is fusion negative.
Knowing if fusions are present in AML is important as both the WHO (5th edition, 2022) and the ICC (2022) classifications define multiple AML subcategories based on rearrangements. Knowing them can help guide therapy choices, patient prognosis, as well as post-treatment monitoring.
“The presence of these rearrangements may preempt the morphologic blast count (diagnostic of AML with <20% blasts), and often conveys important information for prognosis, therapy, and monitoring,” the research team noted in their poster.
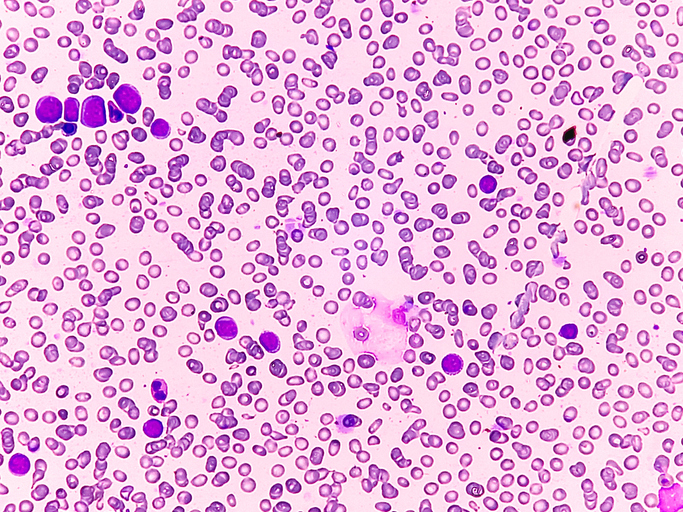
To evaluate the expanded panel, the Michigan Medicine team conducted a five-year retrospective review of all sequenced AML and myeloid sarcoma cases to identify 601 AML cases. Gene fusions were detected in 91 cases (15%), 23 of which were cytogenetically cryptic by karyotype (25% of AML with gene fusions; 4% of total AML cases). Cryptic fusions included rearrangements involving NUP98 and KMT2A, which are known to be difficult to see via karyotype due to their telomeric locations or numerous potential fusion partners.
The RNA assay also identified PML::RARA in two acute promyelocytic leukemia cases that were not evident by cytogenetics, along with other fusions such as CBFB::MYH11, DEK::NUP214, and KAT6A::CREBBP. Additional cases showed suspicious but inconclusive cytogenetic findings, and three cases lacked cytogenetic testing entirely due to inadequate samples or tissue type.
“Disease-defining gene fusions were detected in a significant number of AML cases routinely submitted for Myeloid NGS. In 4% of cases (26% of fusion positive cases), these fusions were cytogenetically cryptic and would not have been detected by karyotype alone,” the researchers noted.
Post noted that two thirds of fusion-positive cases were detected by both the NGS panel and karyotype, but “that also means that one-third were not detected by both.” In cases where NGS detected cryptic fusions, fluorescence in situ hybridization (FISH) was not routinely ordered at the outset. Post noted that “in about two thirds of cases, NGS was the only technique detecting these gene fusions that came through.” The practical challenge, Post said, is that ordering FISH for every possible rearrangement would require “at least 14 break apart probes,” and potentially up to 17 depending on the WHO or ICC classification differences.
Post acknowledged there are some limitations to their assay, noting that some rare fusion partners are not included in the assay design, and certain rearrangements, such as AML with MECOM rearrangement (an enhancer-hijacking event), cannot be detected with the RNA-based fusion panels. In addition, for NUP98 there are about 40 fusion partners and the Michigan panel capture around five, which cover the most common events but not all.
The team also missed one KMT2A rearrangement involving a rare partner not included in the panel. In such situations, alternate methods such as karyotype, break-apart FISH, optical genome mapping, or fusion-agnostic assays, may be required.
Despite these gaps, the findings demonstrate that RNA-based fusion testing complements standard cytogenetics and detects clinically actionable events missed by chromosome analysis alone. “It’s important to know the limitations here, and the limitations are not insignificant, but the performance metrics show that it works in the vast majority of cases,” Post said.