Researchers at the Perelman School of Medicine at the University of Pennsylvania have developed an experimental chimeric antigen receptor regulatory T cell (CAR Treg) to target oxidized low-density lipoprotein (OxLDL) as a potential immunotherapy for coronary artery disease (CAD) driven by atherosclerosis. The preclinical findings, published in Circulation, show that redirecting regulatory T cells to suppress inflammation associated with OxLDL may reduce plaque development in the arteries.
“Our study shows for the first time how CAR T cell technology could be used to treat the underlying cause of the most common form of heart disease, which is the leading cause of death worldwide,” said senior author Avery Posey, PhD, an assistant professor of pharmacology at UPenn. “This preclinical finding represents an important step forward for continuing to expand the impact of CAR T cell therapy to common diseases beyond cancer.”
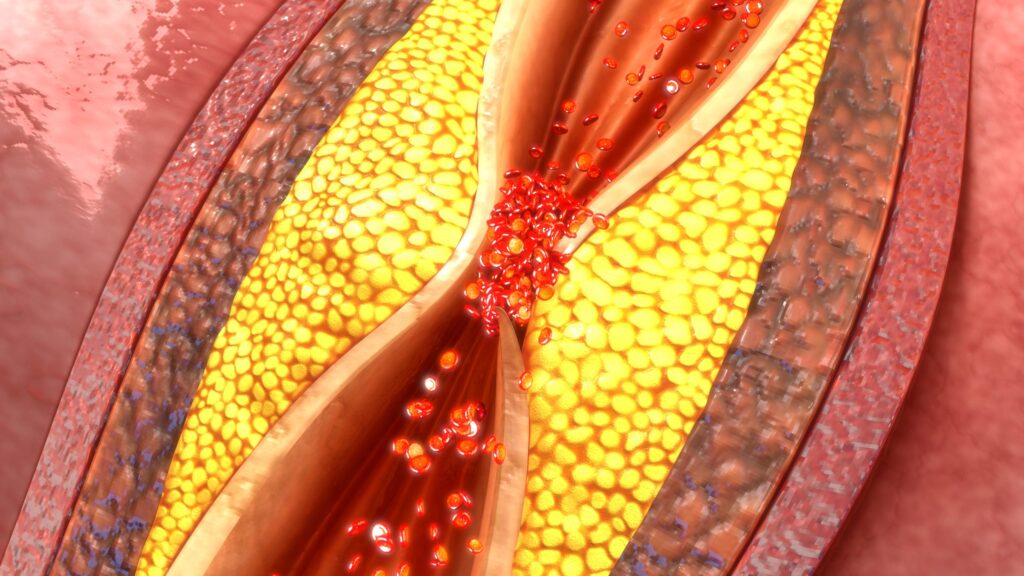
For their study, the researchers focused OxLDL since it is known to be a pro-inflammatory driver of plaque formation. The team then engineered human and mouse regulatory T cells to express a CAR that recognizes an oxidation-specific epitope. “OxLDL is a pro-inflammatory molecule, and that inflammation is what starts atherosclerosis,” said lead author Robert Schwab, MD, a hematology-oncology research fellow at Penn Medicine. “The idea was, if we can get the immune system to see OxLDL and provoke an anti-inflammatory response, it would reduce inflammation and essentially stop the pathogenesis in its tracks.”
The study drew on a trove of prior research demonstrating that OxLDL contributes to endothelial activation, cytokine release, macrophage recruitment, foam-cell formation, and plaque instability. Evidence from earlier studies has shown that antibodies or antibody fragments that block OxLDL can reduce atherosclerotic lesion size in mice and that Tregs, though they are scarce in plaque, can play a role in mitigating atherosclerosis.
Drawing upon this information, the Penn researchers sought to engineer CD4 T cells that would express both FoxP3 and the anti-OXLD CAR via lentiviral vector delivery. This ensured “that all CAR-expressing cells adopted a regulatory phenotype and minimizing the risk of Treg instability or functional plasticity,” the researchers wrote. The engineered cells maintained Treg properties, secreted anti-inflammatory cytokines upon stimulation, and reduced foam-cell formation in vitro.
To determine therapeutic potential of their approach, the investigators developed murine CAR Tregs incorporating mouse FoxP3 and CD28 signaling domains, which they administered to immunocompetent hyperlipidemic mouse model that approximate human OxLDL biology.
Evaluation of the mice 12 weeks after treatment with the engineered Tregs showed they had around 70% less plaque burned compared to the control mice, while showing no disruption to their overall immune function.
CAR T therapies have made a large impact on the treatment of cancer, much of it built on research conducted at UPenn. Both Posey and Schwab have prior experience working in cancer-focused CAR T research under the guidance of CAR T pioneer Carl June, MD.
“Cancer, inflammation, and heart disease go hand-in-hand,” Posey said. “We’re inspired by the potential that this technology developed for cancer could have to help so many people, cancer survivors included.”
Next steps for the Penn team will be to determine whether the CAR Tregs can eliminate established plaques rather than only slowing new plaque development. They also intend to develop a humanized atherosclerosis model to assess the safety and function of human CAR Tregs, in order to understand their persistence and long-term activity in human systems. Based on these findings, UPenn and the researchers have launched Cartio Therapeutics to advance the anti-OxLDL CAR Treg toward clinical testing.