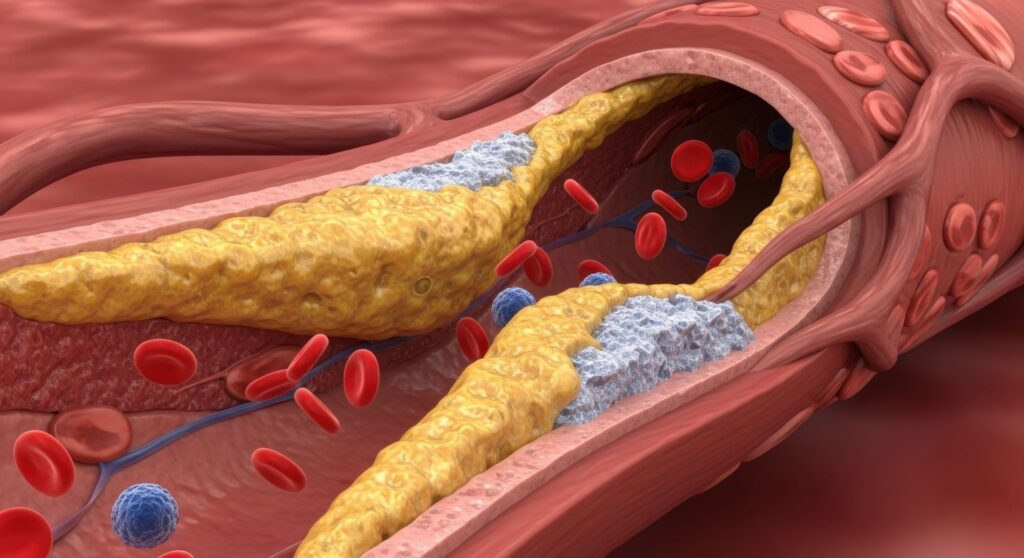
Cardiovascular disease remains the leading cause of mortality worldwide, yet its pathogenesis is not fully understood, hindering the development of effective early diagnostics and treatments. Despite mainstream treatments targeting traditional risk factors such as cholesterol levels, many patients face cardiovascular events. Emerging evidence suggests that chronic inflammation and the gut microbiome contribute to the development of atherosclerosis, thereby helping to identify early markers of the condition in asymptomatic individuals.
Recent findings published in Nature1 show that the gut microbiota-derived metabolite imidazole propionate contributes to atherosclerosis and might be a useful marker of early active atherosclerosis.
Using an unbiased metabolomics approach, the authors first screened atherosclerosis-prone ApoE-knockout (ApoE–/–) mice, which are the most widely used mouse model for the development of atherosclerosis and are characterized by increased total plasma cholesterol levels, for microbial metabolites involved in early atherosclerosis. The gut microbiota-derived metabolite ImP was associated with early-stage disease. ImP is a metabolite resulting from microbial histidine metabolism that has been associated with type 2 diabetes, coronary artery disease, and heart failure2.
Plasmatic levels of ImP were also elevated in two separate cohorts of Spanish and Swedish individuals with subclinical atherosclerosis compared with healthy volunteers and correlated with early-stage atherosclerosis even after adjustment for classical risk factors, including body mass index, fasting glucose, and blood pressure. Moreover, plasma ImP levels were increased in individuals with subclinical metabolically active atherosclerosis, as indicated by increased 18F-fluorodeoxyglucose uptake in arteries, and ImP improved risk stratification when added to conventional cardiovascular markers. As David Sancho, the corresponding author of the study, notes in an accompanying research highlight in Nature Cardiovascular Research3: “What makes this finding clinically significant is that ImP appears to act early in the disease process. This opens the door to earlier detection strategies, particularly in individuals who otherwise be considered low-risk by traditional metrics.”
To explore whether ImP was causally involved in the development of atherosclerosis, ImP was orally administered in atherosclerosis-prone ApoE–/– and LDL receptor knock-out (Ldr–/–) mice. ImP provoked the development of plaque build-up in the aorta and aortic root in both mouse models without altering cholesterol and glucose blood levels. It turned out that ImP supplementation activated pro-inflammatory pathways in macrophages and fibroblasts, involving increased T cell infiltration and expansion of pro-inflammatory monocytes, with the mTOR pathway being a key downstream effector of ImP-induced atherogenic activity. However, blocking the ubiquitously expressed imidazoline receptor I1R with I1R antagonist AGN192403 prevented plaque formation and slowed disease progression, even when mice were fed a high-cholesterol diet. As discussed by the authors, these findings suggest a novel therapeutic potential of combining I1R blockade with cholesterol-lowering drugs to produce a synergistic effect that prevents the development of atherosclerosis, further advancing the potential role of precision medicine in targeting the microbiome for the treatment of cardiovascular disease, particularly in seemingly healthy individuals with subclinical inflammation and atherosclerosis.
These findings highlight that ImP may act as both a marker of early active atherosclerosis and an active driver of atherosclerosis. They also support the potential role of ImP in disease risk assessment and stratification, adding diagnostic value beyond traditional cardiovascular risk factors such as LDL cholesterol, and the potential role of targeting the imidazole propionate-I1R axis in the management of atherosclerosis.
References:
- Mastrangelo A, Robles-Vera I, Mañanes D, et al. Imidazole propionate is a driver and therapeutic target in atherosclerosis. Nature. 2025; 645(8079):254-261. doi: 10.1038/s41586-025-09263-w.
- Molinaro A, Lassen PB, Henricsson M, et al. Imidazole propionate is increased in diabetes and associated with dietary patterns and altered microbial ecology. Nat Commun. 2020; 11(1):5881. doi: 10.1038/s41467-020-19589-w.
- Martini E. Imidazole propionate promotes atherosclerotic plaque formation. Nat Cardiovasc Res. 2025; 4(9):1035. doi: 10.1038/s44161-025-00706-1.