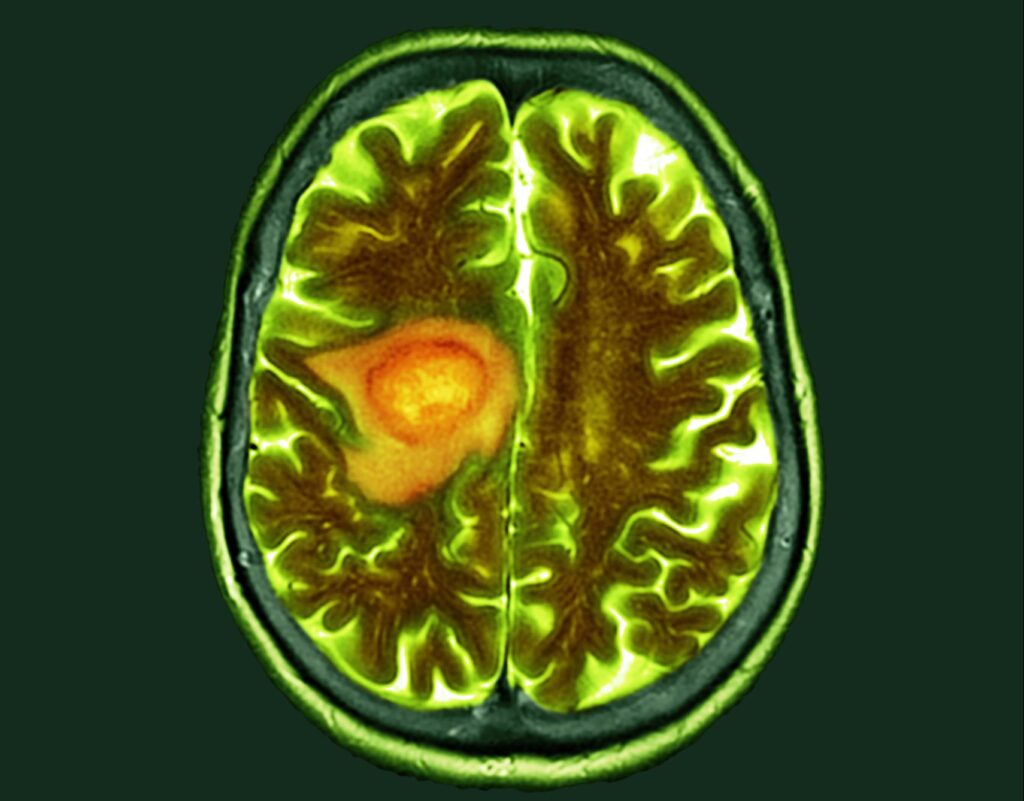
Glioblastoma remains one of the most lethal solid tumors, with median survival measured in months despite surgery, radiation, and chemotherapy. Immunotherapies that transformed treatment for other cancers have repeatedly fallen short in glioblastoma, largely because the tumor microenvironment suppresses nearly every arm of the immune response. Against this backdrop, researchers have been searching for platforms that can both kill tumor cells and disrupt the immunosuppressive ecosystem that protects glioblastoma from attack.
A new preclinical study from Mass General Brigham, published in Nature Cancer, demonstrates that a rationally engineered herpes simplex virus (HSV-1) may provide exactly that combination. The team designed a next-generation oncolytic virus capable not only of targeting glioblastoma cells with precision but also of delivering a coordinated set of immunomodulatory molecules directly into the tumor microenvironment.
“We engineered a safe and traceable oncolytic virus with strong cytotoxic and immunostimulatory activities for glioblastoma immunotherapy,” said senior author Francisco J. Quintana, PhD. “This platform offers a multipronged approach—precise tumor targeting, local delivery of immunotherapeutic payloads, and a built-in safety system to protect normal brain cells.”
Rewriting the rules of oncolytic immunotherapy
Oncolytic viruses have been evaluated for glioblastoma for more than two decades, but most candidates exert limited immunologic effects or fail to overcome the profound immune dysfunction that characterizes the disease. The platform described in this study attempts to shift the paradigm by combining selective oncolysis with deep immune remodeling.
The researchers began by modifying HSV-1 so that it recognizes molecular markers expressed exclusively on glioblastoma cells, blocking viral entry into healthy CNS cells. They then inserted a suite of five immunomodulatory payloads—IL-12, anti-PD1, a bispecific T-cell engager, 15-hydroxyprostaglandin dehydrogenase, and anti-TREM2. Each of these targets a distinct barrier in the glioblastoma microenvironment, from restoring T-cell activation to suppressing myeloid-driven immunosuppression.
To further strengthen tumor control and safety, the virus carries “off-switch” mutations that prevent replication in neurons. It is also PET-traceable: the team incorporated a reporter gene enabling noninvasive monitoring of viral distribution, an increasingly important feature as researchers consider human trials.
Immune reinvigoration and survival benefits
In several preclinical glioblastoma models, a single injection of the engineered virus reshaped the tumor microenvironment within days. The treated tumors showed markedly increased infiltration of cytotoxic T cells and natural killer cells, along with expanded myeloid populations capable of antigen presentation. Exhaustion markers on intratumoral T cells declined, indicating functional rescue. Mice treated with the virus lived significantly longer than controls, supporting the hypothesis that immune remodeling drives durable antitumor activity.
Together, these findings align with a broader shift in neuro-oncology toward combination immunotherapies that target immune suppression at multiple levels. While checkpoint inhibitors alone have been largely ineffective in glioblastoma, combining viral oncolysis with payloads that activate lymphoid and myeloid compartments may help overcome intrinsic and adaptive resistance.
A roadmap toward clinical translation
Safety is the central challenge for CNS-directed viral therapies. The inclusion of non-permissive mutations for healthy neurons, PET-traceable monitoring, and tumor-restricted viral tropism specifically addresses this barrier. The next step, the team notes, is to evaluate safety and antitumor activity in early-phase clinical trials.
Beyond glioblastoma, the modular platform could be adapted for immune remodeling in other solid tumors characterized by similar immunosuppressive landscapes. Each payload is replaceable, allowing the virus to be tailored to distinct tumor ecosystems.
The findings also reinforce growing interest in “multipronged” oncolytic platforms—agents that simultaneously debulk tumors, prime innate and adaptive immunity, and recondition the microenvironment. For glioblastoma, a disease long defined by therapeutic failure, the approach offers cautious but meaningful optimism.