At the 67th American Society of Hematology (ASH) Annual Meeting, researchers from The University of Texas MD Anderson Cancer Center presented new clinical data positioning pivekimab sunirine (PVEK), a CD123-targeting antibody-drug conjugate, as a potential addition to treatment strategies for two aggressive and historically hard-to-treat malignancies: acute myeloid leukemia (AML) and blastic plasmacytoid dendritic cell neoplasm (BPDCN). Unlike many antibodies that rely solely on immune engagement, PVEK delivers a DNA-damaging payload directly into CD123-expressing cells, a design intended to support activity even in chemoresistant disease.
A targeted strategy for CD123-positive leukemias
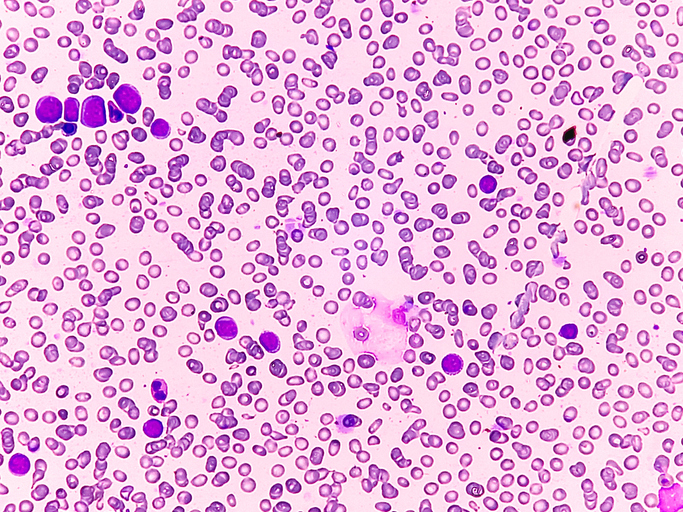
The first study, a Phase Ib/II trial led by Naval Daver, MD, explored whether PVEK could enhance outcomes for older adults with newly diagnosed CD123-positive AML who are ineligible for intensive induction chemotherapy. This population has few curative options, and although venetoclax combined with azacitidine has become a standard low-intensity regimen, treatment failures and resistance remain significant concerns. Because CD123 is frequently overexpressed on leukemia blasts, investigators sought to determine whether adding PVEK to venetoclax and azacitidine could deepen responses without adding prohibitive toxicity.
Among 49 treated patients, the triplet regimen demonstrated high remission rates: over 63% achieved complete remission and nearly 80% reached complete remission with incomplete hematologic recovery. Molecular assessments indicated that most responders were also negative for measurable residual disease, an important predictor of long-term outcomes. The durability of these responses cannot yet be fully assessed, given the relatively short follow-up, but several patients were able to proceed to allogeneic stem cell transplantation, an option often foreclosed to older adults due to disease persistence or treatment intolerance. No unexpected safety signals emerged, suggesting that replacing, not intensifying, cytotoxicity may allow for deeper remissions without increasing risk.
While AML represents a large and genetically heterogeneous disease, BPDCN is rare, highly aggressive, and uniformly expresses CD123, making it an appealing target for PVEK. The Phase I/II CADENZA study, led by Naveen Pemmaraju, MD, evaluated PVEK monotherapy in this population. Early results already indicated high response rates in newly diagnosed patients, but the ASH 2025 presentation focused on an especially challenging subgroup: individuals with BPDCN who also have prior or concomitant hematologic malignancies (PCHM). Historically, this subgroup fares worse than those with de novo BPDCN because the coexisting disease limits marrow recovery and narrows available treatment windows.
Why CD123 targeting matters
The CADENZA abstract provides critical detail on this subgroup, representing roughly one-third of the frontline cohort. These patients were older, with a median age of 73, and many carried concurrent myelodysplastic syndromes or chronic myelomonocytic leukemia. Despite these unfavorable features, PVEK achieved response rates comparable to those in de novo BPDCN. The overall response rate reached 90.9%, with a composite complete response rate of 63.6% and a median overall survival of 17 months—an outcome that rivals or exceeds historic benchmarks for this disease, according to the investigators. Notably, nearly half of the PCHM subgroup was successfully bridged to stem cell transplant, a milestone that illustrates both disease control and tolerability.
Unlike the AML triplet regimen, which leverages PVEK alongside other agents, the BPDCN data reflect the activity of PVEK as a single therapy, highlighting the strength of targeting CD123 in a cancer where the antigen is universally expressed. The ADC’s mechanism, based on an indolinobenzodiazepine pseudodimer payload, is engineered to cause DNA strand breaks without crosslinking, potentially offering a distinct toxicity profile compared with existing cytotoxic approaches. The tolerability profile in the trial was manageable, with adverse events largely consistent with expectations for heavily pretreated patients and with no new safety signals that would preclude continued development.
Looking ahead: Toward registrational pathways
Beyond response rates, both studies contribute to broader discussions in hematology regarding the role of antigen-targeted therapeutics in older or medically complex patients. CD123 has long been recognized as a compelling target, but prior efforts, including immunotoxins and unconjugated antibodies, faced limitations related to off-tumor effects or insufficient potency. The data presented at ASH suggest that PVEK may overcome some of these challenges by combining precision targeting with an optimized payload and dosing strategy.
Still, the path to clinical adoption is not straightforward. Longer follow-up will be needed to determine whether early remissions translate into durable disease control. For AML, randomized studies will be essential to determine whether adding PVEK meaningfully surpasses the current venetoclax–azacitidine standard. For BPDCN, a rare and clinically heterogeneous disease, enrollment and comparative trials may be more difficult, but the CADENZA results provide a strong rationale for continued development.
Taken together, these studies highlight the growing momentum behind antibody-drug conjugates in hematologic cancers and point toward CD123 as a target with therapeutic potential spanning multiple malignancies. Whether PVEK ultimately reshapes treatment paradigms will depend on ongoing trials, but the ASH 2025 results offer cautious optimism for patients facing limited options.