New research from the Sylvester Comprehensive Cancer Center suggests that a virtual program centered on diet and exercise may help patients better tolerate chemotherapy for lymphoma and remain on schedule with their prescribed regimens. Early results of this form of intervention were derived from the Lifestyle Intervention of Food and Exercise for Lymphoma Survivors (LIFE-L) randomized clinical trial, which is evaluating whether lifestyle support delivered during chemotherapy can reduce the side effects from lymphoma therapies that are known to interfere with ongoing, prescribed treatments.
Early findings from LIFE-L will be presented at the American Society of Hematology annual meeting in Orlando this week. The researchers sought to develop and test this intervention spelled out in LIFE-L because as Melissa Lopez, PhD, RDN, said in the press release, “a lot of the work that has been done in the area of lifestyle and oncology has been in the prevention setting or in the survivorship setting after treatment,” and there is limited data on how diet and exercise may influence outcomes during active chemotherapy. Lopez is the first author of the research abstract and a postdoctoral researcher in the Crane lab at Sylvester Comprehensive Cancer Center.
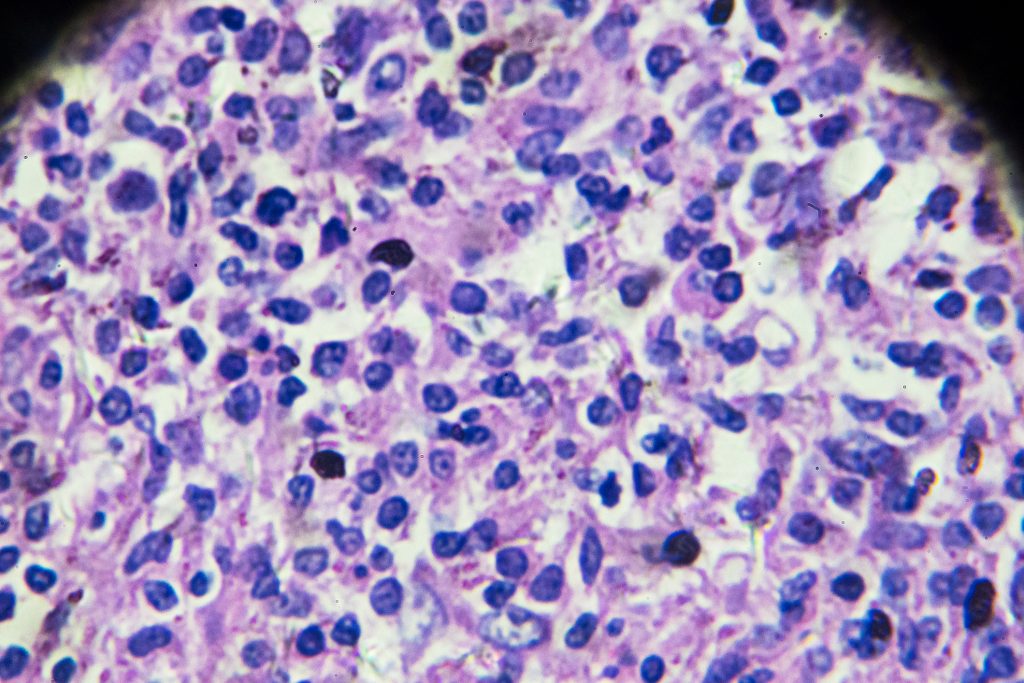
The trial builds on earlier studies in solid tumors which have shown that a structured diet and exercise eases chemotherapy-related symptoms and improve treatment tolerance. The Sylvester team launched their study to find out if similar interventions could have the same positive effects in hematologic malignancies. “While evidence from solid tumors suggests diet and exercise may ease chemotherapy-related symptoms and improve tolerance, these effects remain understudied in hematologic malignancies such as Hodgkin and non-Hodgkin lymphomas,” the researchers wrote.
The LIFE-L trial is a two-arm randomized waitlist-controlled study that is evaluating the effects of a Mediterranean diet and a home-based strength and aerobic exercise regimen in adults receiving six-cycle combination chemotherapy for newly diagnosed Hodgkin or non-Hodgkin lymphomas. Participants were randomized 2:1 to the intervention or waitlist control group prior to the start of treatment. The program consists of individualized weekly remote sessions with a dietitian and an exercise physiologist provided for the duration of chemotherapy treatments. Feasibility for such a program was defined as at least 50% of eligible patients choosing to participate, with retention marked by completion of at least 80% of sessions and satisfaction defined as at least 80% of participants reporting satisfaction with the program.
The study enrolled 72 patients with a median age of 54, comprising 44 in the intervention arm and 28 in the control group. Early study data showed that 81% of eligible patients enrolled, with diet-session attendance reaching 86%, and exercise-session attendance reaching 81%. For the exercise portion of the study, the team first needed to find whether patients were capable of doing the exercises during treatment. “We can offer it all day long, but are people going to want to be a part of it? Are they able to physically and mentally be in the headspace that they want to do this?” Lopez said.
Interim results show that the patients who received the intervention reported lower rates of moderate to very severe side effects such as anxiety, depression, pain, fatigue, and constipation compared with the control group. Physical function in the intervention arm were also better. Handgrip strength averaged 30.2 kg in the intervention group versus 23.2 kg in the control group, and Short Physical Performance Battery gait scores were also higher.
Study assessments were conducted during routine clinic visits at baseline, before treatment cycles three and six, and again four weeks after treatment, which allowed for comparison between the intervention and control groups at multiple times during therapy. Researchers plan to reevaluate outcomes once full trial data are available, including the primary endpoints of chemotherapy relative dose intensity and survival.
The investigators are also examining whether these improvements in adverse symptoms and physical function can help patients stay on schedule and not interrupt their treatment cycles.
“We know that if patients receive less than 85% of their prescribed chemotherapy, there are implications for survival.” said lead researcher Tracy Crane, PhD, associate professor of medical oncology and director of digital health and lifestyle medicine for cancer survivorship at Sylvester. “Our goal with LIFE-L is to show that lifestyle interventions aren’t just for prevention or post-treatment—they can make a real difference during treatment.”