Researchers in Japan at Okayama University and Tohoku University have found a way to improve drug delivery for pancreatic ductal adenocarcinoma (PDAC) by targeting collagen signaling rather than collagen’s physical structure alone. Their method, published in the journal Small, shows that inhibiting discoidin domain receptor 1 (DDR1), a collagen-activated receptor that helps fuels fibrosis, reduces collagen I production and increases the permeability of fibrotic tumor tissue to macromolecular drugs.
“Our findings reveal that collagen signaling, not just its physical density, plays a crucial role in hindering drug delivery,” said senior researcher Hiroyoshi Y. Tanaka, MD, PhD, an assistant professor in the School of Pharmaceutical Sciences at Okayama University. “By inhibiting DDR1, we can interrupt this signaling cascade, loosen the fibrotic barrier, and enable better access for therapeutic agents.”
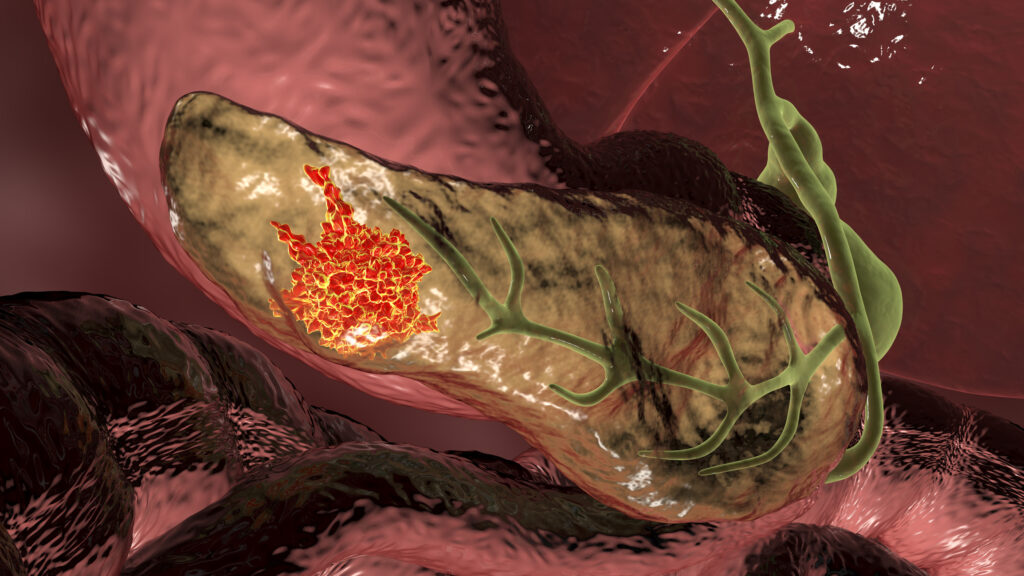
The research was built on current thinking that collagen I, which is abundant in PDAC tumors, physically obstruct penetration of drugs into the tumor. “Fibrosis poses a significant physical barrier to drug delivery, and is particularly problematic for the delivery of macromolecules, such as albumin, therapeutic antibodies, and nanomedicines,” the researchers wrote in their study.
But the research team sought to find if collagen may have other influences beyond physical obstruction. To do this, the researchers used a three-dimensional PDAC fibrotic tissue model constructed from patient-derived pluripotent stem cells (PSCs). To find whether DDR1/2 played a more central role in the generation of the fibrotic barriers they inhibited blocking drug delivery, the team inhibited these receptors within their model.
The data generated showed that “DDR1/2 inhibition diminishes collagen I expression in PSCs to enhance macromolecular delivery. Altogether, the results show in vitro that DDR1-mediated collagen signaling exacerbates the fibrotic barrier and may be targeted to enhance macromolecular drug delivery in PDAC.” Specifically, they found that DDR1, not DDR2, is the primary contributor driving fibrosis.
In addition to clarifying DDR1’s role, the researchers mapped downstream signaling effects, tying DDR1 activity to the PI3K/AKT/mTOR pathway and to alternative mTOR complexes, a connection that could serve as an additional target to reduce fibrotic development.
To verify their findings, the team repeated their permeability assays using a number of macromolecular drugs, including antibodies and nanomedicines, to assess collagen expression changes. They also compared inhibitor effects on canonical and alternative mTOR complexes to confirm the specific pathways involved.
An important finding from this research related to a class of drugs called MEK inhibitors. These drugs block the activity of MEK1 and MEK2, enzymes that are active in the MAPK/ERK pathway that show abnormal activity in PDAC. But past clinical trials applying MEK inhibitors have failed, and this new research could help open the door for them to be effective. “MEK inhibitors exacerbated the fibrotic barrier at clinically relevant doses, an effect that could be reversed by DDR1/2 inhibition,” the researchers wrote.
While these are early results in pre-clinical models, the research is very promising for one of the hardest to treat cancers and one with a dismal five-year survival rate of around 13%. The team now plans to conduct in-human trials to validate if this approach translates to in vitro uses. In addition, a core focus of the research will be on identifying combination therapeutic approaches that target both the fibrotic microenvironment and the tumor itself. They also intend to examine if there are additional collagen subtypes that influence fibrotic development.