The brain has long been regarded as the organ that underlies consciousness and, therefore, as the primary organ in the definition of identity. The symbolic centrality that the brain holds among other organs in the collective imagination is also reinforced, from a physiological point of view, by the role that the brain and the entire nervous system play within the bodily system. In fact, the nervous system is, among various physiological systems, uniquely capable of gathering, processing, and interpreting information from the internal and the external environment and driving coordinated responses across the cardiovascular, endocrine, immune, metabolic, and behavioral domains to maintain physiological balance or “homeostasis.”
Within this system, the vagus nerve holds a central role. As the longest and most widely distributed cranial nerve, it serves as a primary biunivocal communication pathway between the brain and other internal organs. Through bidirectional signaling, the vagus nerve influences heart function, immune activity, digestion, and stress regulation.
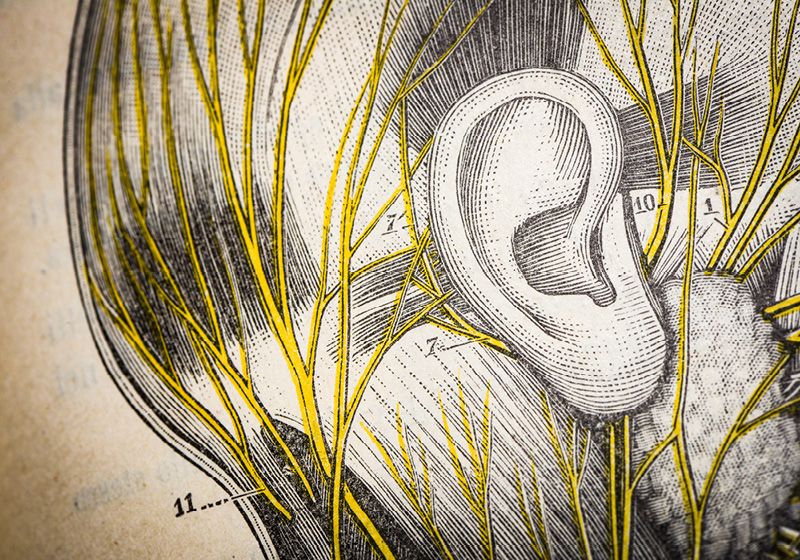
As the vagus nerve is recognized as a key component in the maintenance of body health, the ear, traditionally regarded as the organ responsible for hearing and balance, is now also understood as a key interface to the bodily homeostatic systems, providing a direct access point to vagal pathways connected to the brainstem.
This new understanding has led to growing interest in the development of non-invasive neuromodulation techniques capable of directly modulating vagus nerve activity through targeted electrical signals delivered transcutaneously at the level of the ear.
By offering a non-invasive conduit to the brainstem, auricular vagus nerve stimulation (aVNS) is now emerging as one of the most promising innovative treatment approaches in medicine, enabling clinicians to engage the body’s intrinsic homeostatic systems with a high degree of safety and precision.
The Ear as a Practical Access Point to the Vagus Nerve
Invasive vagus nerve stimulation (iVNS) was the first vagal neuromodulation treatment approach developed. This technique has traditionally required surgical implantation of a pulse generator in a subcutaneous pocket in the infraclavicular region of the chest and was historically approved in the treatment of resistant epilepsy and major depressive disorder. Its invasiveness and cost have more recently driven the development of alternatives aimed at stimulating the vagus nerve without the need for surgery.
Among these non-invasive alternatives, the transcutaneous approach at the level of the tragus of the ear has gained great interest because of its safety and accessibility: aVNS works by targeting the auricular branch of the vagus nerve which lies just underneath the skin here and carries information to the brainstem without directly stimulating the peripheral organs, making it the privileged access way to the vagus nerve.
Preliminary research suggests that aVNS may engage the same neural circuits and achieve similar clinical downstream effects as implantable devices, notably with much higher safety and lower costs for the patients.
Clinical aVNS Evidence and Applications
Cardiovascular Regulation and Blood Pressure Control
One of the fields where aVNS is showing the most promising clinical effectiveness is the cardiovascular space. Let’s take the case of hypertension, one of the most prevalent conditions and most relevant risk factors for major cardiovascular events.
Essential hypertension reflects an autonomic imbalance, where stress-related signaling outweighs vagal regulation. This imbalance is known to contribute to the initiation, maintenance, and progression of hypertension, as well as to the development of hypertension-mediated cardiac and vascular damage. As aVNS has shown robust preliminary efficacy in improving baroreflex sensitivity and vascular function, scientists are further investigating aVNS’s clinical potential in treating hypertension and reducing cardiovascular risk.
A randomized controlled trial published in the Journal of the American Heart Association investigated the effects of a daily 30 minute long aVNS session in otherwise healthy young adults with grade 1 essential hypertension.1 Over three months, the treatment group showed a progressive and statistically significant reduction in both systolic and diastolic blood pressure compared to placebo, without major adverse events.
These results suggest that aVNS might be a potential safe nonpharmacological treatment approach for hypertension management in a relatively young population where stress-related nervous system signaling often plays a central role.
Chronic Conditions
Another set of pilot clinical studies have shown how aVNS could ameliorate chronic conditions potentially through regulation of the inflammatory response and the autonomic tone (the balance between the sympathetic and parasympathetic branches of the nervous system). A paradigmatic case is given by the clinical efficacy shown in post-viral syndromes.
These syndromes, which have come into the spotlight after the COVID-19 pandemic, are often characterized by multi-system symptoms that are often resistant to conventional care. Persistent fatigue, cognitive difficulties, dizziness, sleep disturbances, gastrointestinal symptoms, and palpitations are among the hallmark features of post-viral syndromes such as Long COVID, where evidence increasingly points to autonomic dysregulation, namely an alteration in the balance between sympathetic and parasympathetic nervous system activity, as the main underpinning pathogenetic driver.
A pilot study evaluated aVNS as a potential intervention for Long COVID–related impaired regulation of the autonomic nervous system.2 The results demonstrated marked and statistically significant reductions in symptom burden, including fatigue and depression, and improvements in functional parameters such as grip strength and oxygen saturation after 10 aVNS sessions. Notably, IL-1 receptor antagonist levels rose by roughly 185 percent over the treatment period, suggesting modulation of immune signaling.
Another more recent study conducted in female patients with Long COVID, which instead focused on the cognitive aspects of the syndromes, showed that a 10-day aVNS intervention significantly improved various cognitive functions, and improvements were maintained at 1-month follow up.3
These and other findings support aVNS as a mechanistically distinct therapeutic treatment approach in Long COVID and post-viral syndromes with potential long-term retention of benefits.
Beyond Clinical Treatment
Many other studies have also successfully explored potential effectiveness of aVNS in neuropsychiatric conditions such as fibromyalgia or disorder of consciousness by mainly levering the effect of the technology on central neuroplasticity and systemic inflammation.4,5
However, the potential of aVNS goes beyond the clinical space and emerging evidence suggests that aVNS could also be effective in promoting health by improving cardiovascular fitness and promoting neuro-enhancement effects. Multiple clinical studies conducted in healthy volunteers indeed showed how aVNS improved in heart rate variability, markers of cardiovascular fitness, and cognitive performance. As an example, a pilot randomized study conducted in typically developing young adults showed that aVNS paired with reading selectively enhanced memory-based recall after just one session.6
The effect on cognition is linked to the neuromodulation of specific nuclei in the brainstem which, in turn, would influence widespread subcortical and cortical brain regions involved in attention, cognition, and emotional control.
Clinical Integration and Future Directions
While large-scale trials will be essential to confirm results from very promising pilot data, refine stimulation protocols, and better define the patient populations that might benefit more out of this new treatment approach, aVNS is emerging as a new safe and promising treatment strategy that can be easily combined with other treatment modalities across different specialties and, more broadly, a paradigm shift in how medicine approaches neural regulation and overall disease management.