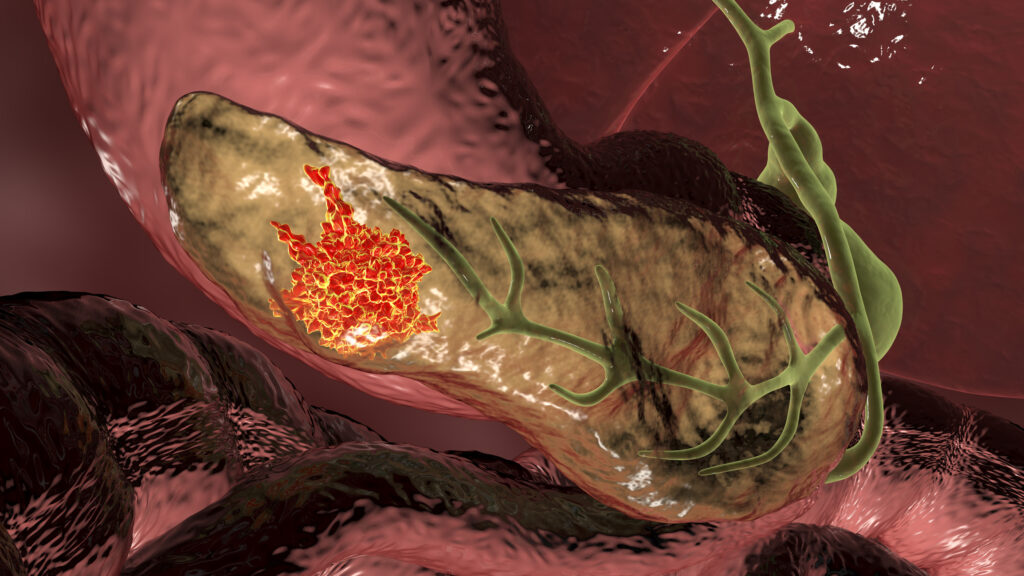
Researchers at Cold Spring Harbor Laboratory have developed a potential new therapeutic strategy for pancreatic ductal adenocarcinoma (PDAC) addressing a newly characterized circuit that promotes aggressive tumor growth. In their study, published in Molecular Cell, the Cold Spring team reported on the development of an antisense oligonucleotide (ASO) designed to disrupt alternative splicing of Aurora kinase A (AURKA), which essentially short circuits a three-component loop involving AURKA, the splicing factor SRSF1, and the transcription factor MYC.
“Our theory was that some of the changes caused by increased levels of SRSF1 were playing a role in the accelerated tumor growth we were seeing,” said lead author Alexander Kral, a graduate student at Cold Spring. “We homed in on a molecule we thought could be an important driver of AURKA. We found it’s part of a complex regulatory circuit that includes not only AURKA and SRSF1, but another key oncogene called MYC.”
The discovery springs directly from prior Cold Spring Harbor research published in 2023 showing that SRSF1 promotes PDAC tumor development and is transcriptionally upregulated by MYC. By revisiting splicing datasets from that research, the investigators identified an exon-inclusion event in the 5′ untranslated region of AURKA controlled by SRSF1. This finding connected earlier observations that MYC induces AURKA transcription and that AURKA stabilizes MYC protein.
“We previously reported that SRSF1 promotes PDAC progression, and SRSF1 expression is upregulated via MYC-driven transcriptional activation,” the researchers wrote. Together with published evidence that AURKA positively regulates MYC and SRSF1 post-translationally, these insights guided the identification of a closed SRSF1–AURKA–MYC circuit.
PDAC treatment today relies on surgery, chemotherapy, and radiation, with surgery possible in only a minority of patients. Most existing therapies today target the KRAS oncogene, but their success has been very limited. PDAC remains one of the most lethal of all solid tumors a five-year survival rate between 10% and 13%.
“It is therefore critical to identify additional pathways PDAC cells use to evade KRAS inhibition,” the researchers wrote. Targeting MYC or SRSF1 directly has proven difficult because of their cellular roles and lack of conventional druggable domains, while AURKA kinase inhibitors have shown limited efficacy.
ASOs are short, synthetic strands of nucleic acids designed to bind specific RNA sequences. In this study, splice-switching ASOs were used to alter how AURKA pre-mRNA is spliced in the nucleus, rather than degrading the RNA. This approach was chosen because AURKA overexpression in PDAC depends on tumor-specific inclusion of exon 2 in the 5′ UTR, a process driven by SRSF1. By forcing exon skipping, the ASO reduces AURKA mRNA accumulation and protein production, destabilizing MYC and lowering SRSF1 levels. “Modulating 5′ UTR splicing with splice-switching antisense oligonucleotides (ASOs) collapses the oncogenic circuit, reducing PDAC cell viability and triggering apoptosis,” the researchers noted.
The ASO was designed based on sequence features surrounding AURKA exon 2 and tested in PDAC cell models. Several ASOs induced exon 2 skipping and reduced AURKA expression without relying on RNA degradation. One of the developed candidates, however, collapsed the entire oncogenic circuit, which reduced tumor cell viability and induced apoptosis, or programmed cell death.
“It’s like killing three birds with one stone,” said senior author Adrian Krainer, PhD, a professor at Cold Spring Harbor. “SRSF1, AURKA, and MYC are all oncogenes contributing to PDAC progression. Just by targeting AURKA splicing with our ASO, we see the loss of these other two molecules as well.”
While the research is in its earlier stages, the potential clinical implication are significant. If developed into an approved drug, the strategy of targeting AURKA splicing with an ASO could add a new class of targeted therapy for PDAC, and could potential be used alongside KRAS inhibitors or chemotherapy to limit treatment resistance. The selectivity of splice-switching ASOs may reduce toxicity by sparing normal AURKA isoforms and the team noted that this approach could also be used to treat other cancers that have high AURKA expression.
Next steps for the Cold Harbor team is work to refine the ASO and use it for additional preclinical studies. “Potential clinical applications are still a long way off,” Krainer said, but added that his lab is continuing to optimize the molecule, following a path similar to earlier ASO development that led to Spinraza, the first FDA-approved treatment for spinal muscular atrophy.