A research team led by investigators at the Mass General Brigham Cancer Institute has developed a liquid biopsy test that can accurately stratify patients with small cell lung cancer (SCLC) based on their likelihood to positively respond to Amgen’s Imdelltra (tarlatamab). These findings, published today in Cancer Discovery, could represent a major step forward in diagnosis and treatment for a form of lung cancer with limited treatment options.
“Our work may help predict which patients with SCLC are likely to respond to tarlatamab and potentially other antibodies targeting DLL3, many of which are in development,” said Justin Gainor, MD, program director of the Center for Thoracic Cancers at the Mass General Brigham Cancer Institute. “It also has potential implications for other cancers that express DLL3 as they become more aggressive and for the field of antibody-directed cancer therapies.”
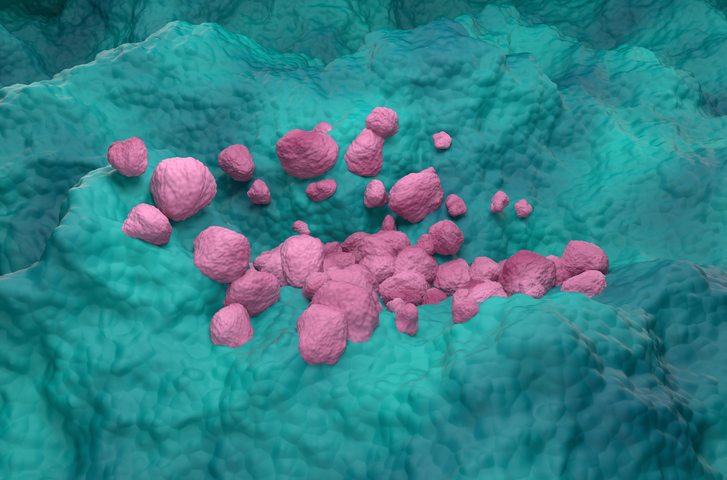
SCLC is an aggressive neuroendocrine cancer characterized by fast growth and early metastasis, meaning most patients are at an advanced disease stage at the time of diagnosis. While first line treatment with platinum-based chemotherapy often achieves a strong initial response, most patients see recurrence within a year. Unlike non-small cell lung cancer (NSCLC), for which there are multiple targeted therapies available, treatment options for relapsed SCLC are limited and clinical outcomes tend to be poor.
In late 2025, the FDA granted approval to tarlatamab for the treatment of patients with extensive-stage SCLC who have experienced disease progression after chemotherapy, expanding treatment options to this patient population. However, more than half of patients treated with tarlatamab experience further disease progression within six months and there yet no validated biomarkers available for patient selection.
Tarlatamab targets the delta-like ligand 3 (DLL3), a protein that is expressed on the cell surface of multiple neuroendocrine tumors including SCLC. To date, efforts to identify predictive biomarkers for tarlatamab have focused on immunostaining approaches looking at DLL3 expression. However, this biomarker is expressed in up to 95% of tumor samples.
In the current study, Gainor and colleagues looked at circulating tumor cells (CTCs) to quantify DLL3 expression in the bloodstream rather than in a tumor biopsy. Using single-cell RNA sequencing, the team identified patients with high or low DLL3 expression levels and showed that these expression patterns were highly predictive of a successful response to tarlatamab.
To achieve this, the researchers used a novel method of CTC enrichment adapted to the unique features of SCLC cancer cells. While enrichment strategies typically rely on the expression of the epithelial cell adhesion molecule (EpCAM) or the larger size of tumor cells, SCLC cancer cells are characterized by their small size and express low or no levels of EpCAM. In contrast, their enrichment method, currently under development by medical technology company TellBio, used microfluidics and magnetically conjugated antibodies to remove normal blood cells from the sample and enrich it in CTCs.
“Isolating cancer cells from the blood has tremendous potential to guide immune-related cancer therapies, and our group has created cutting edge bioengineering technologies for purification of these circulating tumor cells,” said Daniel A. Haber, MD, PhD, director of the Krantz Family Center for Cancer Research at the Mass General Brigham Cancer Institute.
In a cohort of 20 SCLC patients, the blood test showed 85% sensitivity and 100% specificity at predicting clinical benefits of tarlatamab based on DLL3 expression levels before treatment. Among patients who initially responded but later developed treatment resistance, the researchers identified two groups: The first one were patients whose tumors lost expression of DLL3, and the second were patients who showed signs of T cell dysfunction despite continued expression of DLL3.
These results will need to be validated in a larger clinical trial to confirm the predictive value of DLL3 expression in CTCs, as well as find the optimal cutoff point for patient stratification. With ongoing efforts to expand the use of tarlatamab to first-line SCLC treatment, as well as to other types of neuroendocrine tumors, this liquid biopsy test could provide a critical tool for patient stratification. Given the risk of cytokine release syndrome, which mandates hospital admission for all patients receiving their first two doses of tarlatamab, the blood test could also help prevent any unnecessary risks for patients who are unlikely to respond.