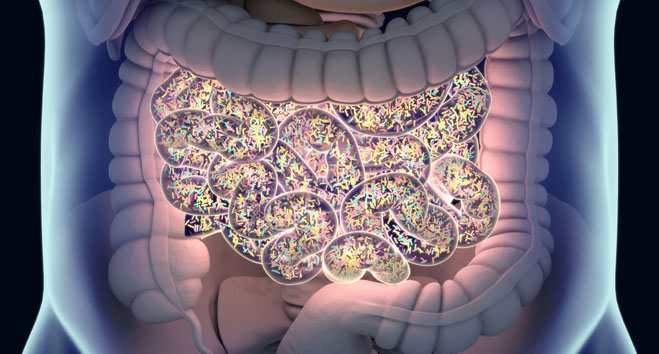
Changing the gut microbiome of patients with kidney, lung or skin cancer using fecal microbiota transplantation (FMT) can help improve outcomes and slow progression when combined with immunotherapy.
Results from three studies published in Nature Medicine show a combination of FMT and immunotherapy and/or other cancer drugs significantly improved outcomes for patients.
The researchers believe stool transplantation in the form of FMT reshapes the gut microbiome in a way that favors anti‑tumor immunity and reduces immunosuppressive signals, rather than by simply adding good bacteria in place of bad.
Two papers looked at patients with metastatic kidney cancer, one called PERFORM was a Phase I trial including 20 patients, led by Saman Maleki, PhD, at Western University and Verspeeten Family Cancer Centre in Ontario, and TACITO was a randomized Phase II trial including 50 patients, led by Gianluca Ianiro at the Università Cattolica del Sacro Cuore and Fondazione Policlinico Universitario in Rome.
The PERFORM study tested whether FMT from healthy donors, given as capsules at the start of treatment, could safely change the gut microbiome and improve responses to two immune checkpoint inhibitors ipilimumab and nivolumab in people with metastatic kidney cancer.
The results showed around 50% of patients had an objective response to FMT plus immunotherapy, and two had a full response. Those who responded well to the combination therapy had less immune related side effects than those who did not.
The TACITO trial tested whether stool from patients who had long‑lasting complete responses to immunotherapy could improve outcomes when added to the current standard drug combination for patients with metastatic kidney cancer, which consisted of the checkpoint inhibitor pembrolizumab plus axitinib, a targeted cancer drug.
The results showed that median progression‑free survival improved from nine months with placebo to 24 months with responder‑donor FMT plus pembrolizumab and axitinib. The researchers also showed that the objective response rate increased from 32% in the placebo group to 52% with FMT, without obvious additional safety concerns.
“Our working hypothesis was that transplanting a ‘favorable’ gut microbiota could enhance response to immunotherapy,” said Ianiro in a press statement. “TACITO is the first randomized trial worldwide to compare immunotherapy outcomes following FMT from immunotherapy responders versus placebo.”
The final study, the Phase II FMT-LUMINate trial, led by Arielle Elkrief, MD, at the University of Montreal, enrolled two groups of patients starting their first treatment for advanced cancer, 20 with non‑small cell lung cancer and 20 with advanced melanoma skin cancer. All patients received a single course of stool capsules from healthy donors and then began standard immune checkpoint inhibitor therapy with pembrolizumab alone for lung cancer, or ipilimumab plus nivolumab for melanoma.
Tumor shrinkage was seen in 80% of lung cancer patients and 75% of melanoma patients, which is higher than typical results with immunotherapy alone. FMT appeared safe in the lung cancer group, but combining FMT with ipilimumab plus nivolumab for melanoma led to frequent serious side effects especially when donors were rich in Prevotella‑type bacteria.
Together, these three trials show that changing the gut microbiome with FMT can meaningfully boost the effectiveness of immune‑based cancer treatments. They provide evidence that FMT can increase response rates and prolong progression‑free survival in metastatic kidney cancer, lung cancer and melanoma, while remaining feasible and mostly safe.