A clinical study involving over 800 participants has shown that targeting neuromodulation treatments to a specific brain region involved in Parkinson’s disease can increase their efficacy up to 2.5-fold. Published today in Nature, these findings reveal the central role that the somato-cognitive action network (SCAN) brain region plays in Parkinson’s, uncovering its potential as a diagnostic biomarker as well as a novel treatment target.
“This work demonstrates that Parkinson’s is a SCAN disorder, and the data strongly suggest that if you target the SCAN in a personalized, precise manner you can treat Parkinson’s more successfully than was previously possible,” said Nico U. F. Dosenbach, MD, PhD, professor of neurology at Washington University School of Medicine. “Changing the activity within SCAN could slow or reverse the progression of the disease, not just treat the symptoms.”
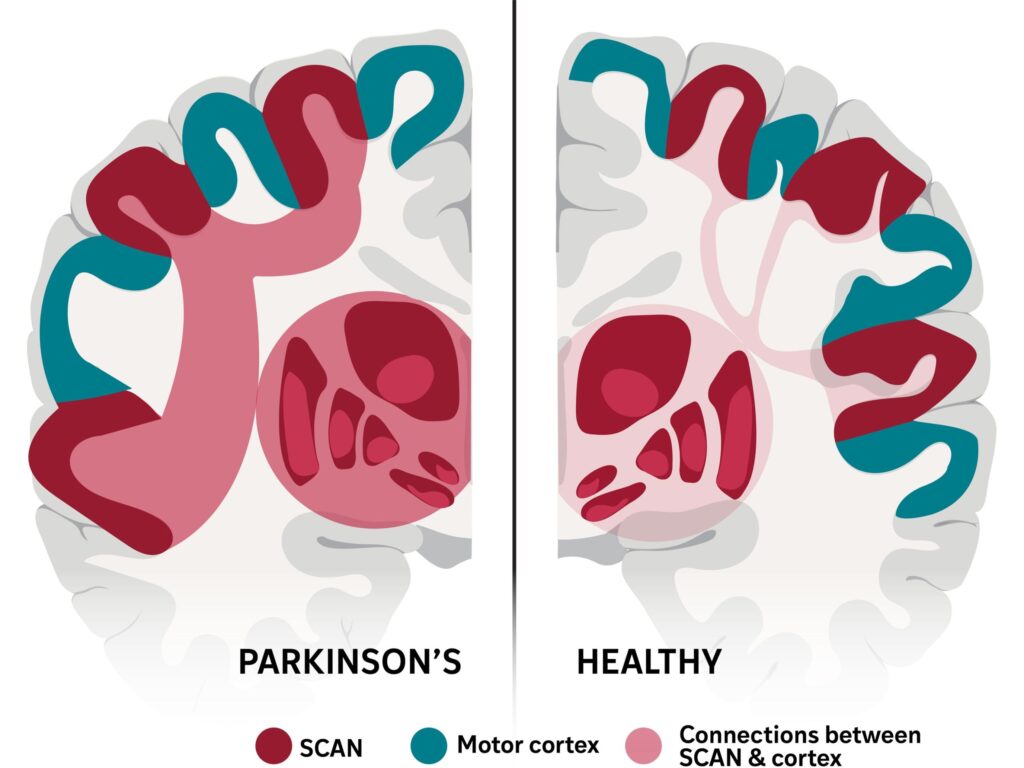
Dosenbach and colleagues had previously reported the discovery of the SCAN region, a brain network found within the motor cortex that is responsible for turning thoughts into movement and receiving feedback on the resulting actions. Since many symptoms of Parkinson’s disease affect motor abilities, the WashU Medicine team set out to study the role of SCAN on this neurodegenerative condition in collaboration with scientists from Peking University in China.
The study analyzed brain imaging data from 863 participants, including individuals diagnosed with Parkinson’s disease as well as healthy controls and patients with different motor disorders including tremors, dystonia and amyotrophic lateral sclerosis (ALS). Results showed that patterns of hyperconnectivity between SCAN and the subcortical region—involved in emotion, memory and motor control—were unique to Parkinson’s patients.
Among Parkinson’s patients, the study included individuals treated with deep-brain stimulation (DBS), transcranial magnetic stimulation (TMS), MRI-guided focused ultrasound stimulation (MRgFUS), and levodopa medication. Across all four groups, patients who responded well to treatment showed signs of reduction in this hyperconnectivity, returning to normal activity levels.
“For decades, Parkinson’s has been primarily associated with motor deficits and the basal ganglia,” said Hesheng Liu, PhD, professor at Peking University. “Our work shows that the disease is rooted in a much broader network dysfunction. The SCAN is hyperconnected to key regions associated with Parkinson’s disease, and this abnormal wiring disrupts not only movement but also related cognitive and bodily functions.”
The team then used TMS to selectively and non-invasively stimulate the SCAN brain region in a small cohort of Parkinson’s patients. Out of 18 individuals who received treatment targeted to SCAN, the response rate was 56% after two weeks. In comparison, the group who received treatment targeted to adjacent brain areas had a 22% response rate, translating to a 2.5-fold efficacy increase.
Although Parkinson’s patients generally respond well to levodopa medication at first, its benefits often decrease over time; neuromodulation techniques are often used at this point. DBS has been the most successful neuromodulation technique, but less than 10% of patients are eligible to receive this invasive treatment that requires brain surgery. Boosting the efficacy of non-invasive techniques that rely on magnetic or ultrasound stimulation could therefore have a large impact on the remaining 90% of patients.
“With non-invasive treatments, we could start treating with neuromodulation much earlier than is currently done with DBS,” said Dosenbach.
Ultimately, these findings have the potential to redefine the neurological basis of Parkinson’s, moving away from conceptualizing it as a complex collection of neurological and motor symptoms and instead focusing on the underlying brain network dysfunctions. Future work will involve clinical trials evaluating the efficacy of non-invasively stimulating the SCAN region to treat Parkinson’s—these studies will be undertaken by Turing Medical, a WashU startup co-founded by Dosenbach.