When standard chemotherapy fails in young men with germ cell tumors, options become limited and often grueling. High-dose chemotherapy can offer a second chance at durable remission, but for many, it comes at the cost of significant toxicity without long-term benefit. A new study published in the Journal of Clinical Oncology suggests that a simple blood test could help identify which patients are most likely to benefit from such intensive therapy.
Investigators from the Princess Máxima Center for Pediatric Oncology, in collaboration with colleagues in Italy and Slovakia, analyzed circulating tumor DNA (ctDNA) in young adults with relapsed or refractory germ cell tumors. Their goal: determine whether fragments of tumor DNA in blood could predict treatment response and survival, and ultimately support more individualized decision-making.
Moving beyond one-size-fits-all salvage therapy
Testicular germ cell tumors are the most common cancer in men aged 15 to 35. While most patients respond well to first-line platinum-based chemotherapy, about one in ten young adults experiences relapse or inadequate response. High-dose chemotherapy is frequently offered in this setting, yet approximately half of these patients ultimately die despite treatment.
The study evaluated blood samples from 69 patients receiving high-dose chemotherapy and 26 patients receiving standard-dose chemotherapy. Using shallow whole-genome sequencing, the researchers measured tumor fraction (TF)—the proportion of circulating DNA derived from tumor cells—and assessed copy number alterations (CNAs), structural changes in tumor DNA. Results were compared with miR-371a-3p, a circulating microRNA that has emerged as a sensitive biomarker for detecting active germ cell tumors.
Tumor fraction as a prognostic signal
Tumor fraction exceeded the detection threshold in 75% of patients treated with high-dose chemotherapy, indicating measurable ctDNA in most cases. Importantly, a high tumor fraction was strongly associated with worse outcomes in both the high-dose and standard-dose groups. Patients with elevated tumor fraction experienced significantly shorter progression-free survival and overall survival.
This finding positions tumor fraction as a potentially powerful prognostic biomarker. In contrast to miR-371a-3p—which proved highly informative for detecting the presence of disease but not for predicting survival—tumor fraction provided risk stratification relevant to long-term outcomes.
Interestingly, the data also suggest that high-dose chemotherapy may be more effective than standard therapy in patients with high tumor fraction, indicating a possible role for ctDNA profiling not only in prognostication but also in therapeutic selection.
Genomic alterations and histologic risk
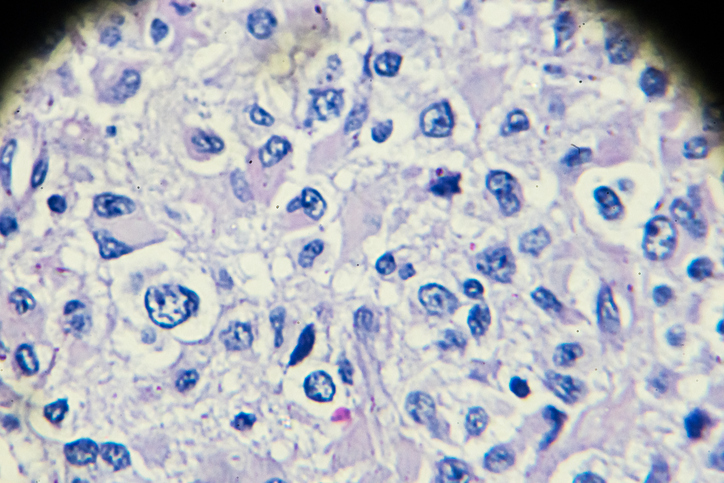
Beyond tumor fraction, specific genomic alterations were associated with poor prognosis. Patients with a higher frequency of 3p gain, 9q and 11q gains, and 6q loss showed worse survival outcomes, particularly in the high-dose chemotherapy group. These copy number alterations may reflect underlying tumor biology that confers chemoresistance.
The study further identified associations between histologic subtype and genomic patterns. Tumors with extra-embryonic histology, such as yolk sac tumor and choriocarcinoma, demonstrated distinct CNA profiles and were linked to inferior survival. This reinforces the biological heterogeneity of germ cell tumors and highlights how liquid biopsy could capture clinically meaningful differences beyond conventional pathology.
Implications for precision oncology
Incorporating ctDNA analysis into the management of relapsed germ cell tumors could address a major clinical dilemma: whether to initiate a final, highly intensive course of chemotherapy in patients with limited life expectancy and uncertain benefit.
The authors conclude that analysis of circulating tumor DNA provides “valuable prognostic information” in germ cell tumors that recur or do not adequately respond to standard chemotherapy. These minimally invasive biomarkers may help refine risk stratification and support decision-making about high-dose therapy, particularly in scenarios where quality of life considerations are paramount.
From a precision medicine standpoint, the approach aligns with broader trends across oncology: using molecular data from blood to guide treatment intensity, avoid futile toxicity, and identify new therapeutic targets. Copy number alterations identified through ctDNA may also point toward future biologically informed interventions that are less toxic than current salvage regimens.
Next steps
Before clinical implementation, these findings must be validated in larger, prospective cohorts, including adolescents and children with germ cell tumors. The research team plans to expand the analysis through international collaboration.
If confirmed, ctDNA-based profiling could become part of routine assessment in relapsed germ cell tumors, helping clinicians tailor treatment strategies based not only on clinical parameters but also on real-time tumor biology.
For a patient population in which decisions about high-dose chemotherapy often carry profound consequences, a blood test that clarifies prognosis and therapeutic value would represent a meaningful advance in precision oncology.