When Peter Nguyen was a graduate student at Rice University, he first encountered synthetic biology while mentoring undergraduates for the International Genetically Engineered Machines (iGEM) competition. He knew he had found his topic right then, and he has never looked back since. Currently, he works in James Collins’ laboratory at the Wyss Institute at Harvard University—one of his notable projects is developing smart fabrics that integrate cell-free sensing systems with computational readout technologies.
Cell-free Systems Run Biological Reactions
Peter Nyugen, a synthetic biologist at Wyss Institute, works on freeze-dried, cell-free technologies for various applications.
Wyss Institute, Harvard University
Most synthetic biology projects involve genetically manipulating living cells, but this traditional approach has a lot of drawbacks. Researchers need to edit and handle living cells, which result in workflow bottlenecks and require enhanced safety protocols. The Collins lab works with cell-free synthetic biology systems instead. “You can take a cell, you can open it up, so that you have all the insides of the cells,” explained Nguyen. “It’s not able to replicate anymore because there’s no cell left, but you have the innards of the cells—they’re still able to actually do synthetic biology for a while. So, it can replicate DNA, it can produce proteins, but it’s kind of a one-shot deal.”
Taking this concept one step further, the team freeze dried this cell-free mix into a powder. “A year later, you can come back to that powder, add water and your DNA, and all the components in that cell-free reaction are still active…and they’ll run that genetic program that you put in, which was very shocking to us,” said Nguyen.
A New Era of Wearable Biosensors
With this freeze-dried system, Nguyen and his team were looking into several applications, a primary one being diagnostics on a piece of paper. “You could add a drop of blood onto that piece of paper [containing the cell-free powder]; that water in your sample would activate the reaction, and then it would analyze what’s in the blood to see, okay, you have malaria, and it’ll light up a different color. And all of this is freeze dried on a piece of paper that’s like the size of a stamp.” The Collins team first demonstrated Ebola virus detection on such sensors about a decade ago.1
Next, Collins and Nguyen wanted to take diagnostics to the source by integrating their technology into wearables. “Fundamentally, our clothing is almost like one of the most ancient technologies we have to shelter us from the environment,” said Nguyen. “It’s almost like a second skin that you created using technology… but we’ve lost the sensing ability that you normally have when you have human skin.”
The skin responds to stimuli, serving as an indicator of any problems. Nguyen wondered if they could create clothing that is responsive and connected to a diagnostic network. He knew they needed to integrate biological computation into wearable textiles.
After screening several fabrics, the team put their freeze-dried, cell-free systems into a compatible fabric that didn’t interfere with the cell-free reactions. Although the system worked fine as a proof-of-principle diagnostic, there were technical challenges, such as heat-driven evaporation, to be overcome. After more than a year of optimizing it, Nguyen finally had a system that worked reliably.
A Sensor-Integrated Mask That Detects SARS-CoV-2
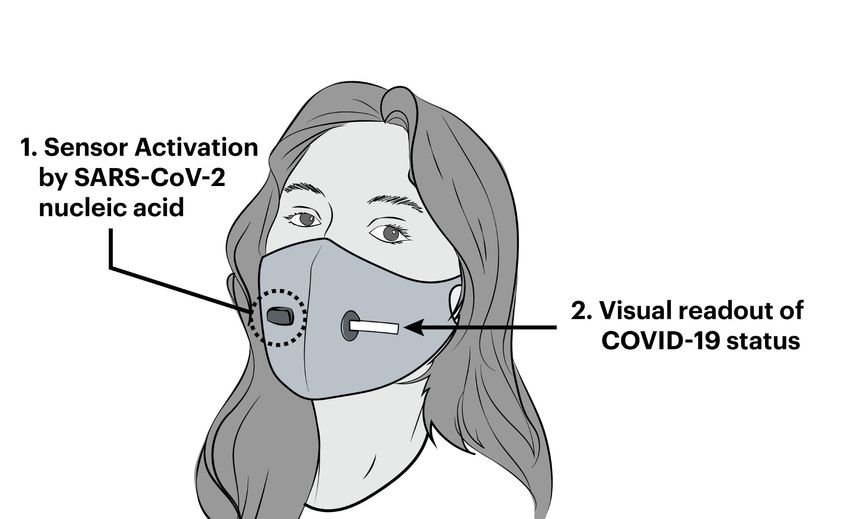
A prototype face mask incorporates freeze-dried cell-free synthetic biology reactions for COVID-19 detection from breath aerosols.
Wyss Institute, Harvard University.
During the COVID-19 pandemic, while work on other experiments stalled, the team saw an opportunity to solve a real-world problem right away. They were already working with wearables, so they decided to adapt their tech to detect the SARS-CoV-2 virus. At that time, doctors were triaging patients, and they didn’t even know if people had COVID-19, so they couldn’t admit them into the specific ward. As qPCR results took up to a week, there was no easy workaround to this problem. Nguyen and his team decided to develop a face mask for rapid COVID-19 diagnoses.
“[The patients are] in the waiting room, or they’re waiting to get admitted in—they’re wearing a mask anyway. And the mask on the inside is being covered with viral particles, right? Is there a way to use that sample? That way, you don’t have to actually wait for an analysis. You do the analysis while you’re breathing into the mask,” he said.
The team successfully built a facemask detector, which was modular and relatively easy to use.2
“It could detect whether or not you had COVID-19 as well as the WHO-approved qPCR method that requires a laboratory. And all you have to do is wear it and breathe in it for an hour,” said Nguyen.
Smart Fabrics: Wearable Synthetic Biosensors Meet Electronics
Once the team had a synthetic biology circuit that worked with fabrics, they could technically build wearable biosensors to detect any pathogen. But Nguyen knew they needed to develop this further. For instance, if one gets hit by a splash of blood with Ebola, the sensor will change color from orange to purple and detect Ebola DNA in it. But the practical issue remains that the user might not notice a color change in one spot on their body right away.
For effective real-time detection, Nguyen wanted to integrate this system into a computational network. “We ended up integrating fiber optics into a fabric. So now this fabric—it’s a woven fabric—has fiber optics woven into it. And it has freeze dried synthetic biology reactions added to it. And so now, when it changes color, we added in a fluorescent reporter instead,” said Nguyen. “The fiber optics can actually detect that light change, and now you have basically a textile that’s constantly probing to see if there’s any light change in these reaction reactors. And once it actually detects a light change, it will send a signal to your cell phone, and you get a cell-phone message saying that we detected HIV DNA that has activated a sensor on your right arm, for example. And so, at that point, we had our system flushed out—it was working beautifully.” The team tested different sensors to detect Ebola, HIV, and chemical warfare agents with this system.
Nguyen acknowledged that one drawback of this technology is that it is a one-and-done system. “It’s exactly like ramen: You open the package, you have everything freeze dried, [and] you put it in. Once you make ramen, you can’t put it back in the package, and so, it’s kind of the same issue with our system.” While synthetic biologists have yet to figure out a way to work with reusable sensors, another wish list item for Nguyen is to develop a multiplexed version of the sensors where a single fabric could warn the user of multiple threats in real time.
While Nguyen and his team work on advanced prototypes, the current version of their wearable system, along with a walkthrough of how they designed it, is on display at the MIT Museum in Boston.

