Lung tumors can undermine the immune system long before immune cells reach the tumor, according to new research from investigators at the Icahn School of Medicine at Mount Sinai. Their study, published online in Nature, shows that cues from the lung cancer tumors provide a “first hit” on myeloid progenitors (precursors of macrophages) in the bone marrow, which dampens interferon response and promotes immunosuppression. Once they reach the tumor, a “second hit” cements their pro-cancer role.
“This work changes the way we think about the timing of immune suppression in cancer,” said lead author Samarth Hegde, PhD, a postdoctoral fellow in the lab of Miriam Merad, MD, PhD. “Our findings show that some of these immune cells are already being reprogrammed in the bone marrow, long before they ever reach the tumor.”
This systemic reprogramming involves the transcription factor NRF2, a stress-response regulator previously implicated in cellular detoxification. This new finding shows how NRF2 primes bone marrow myeloid progenitors in response to tumor-derived inflammation, pushing them toward an immunosuppressive roles that allows cancer to thrive.
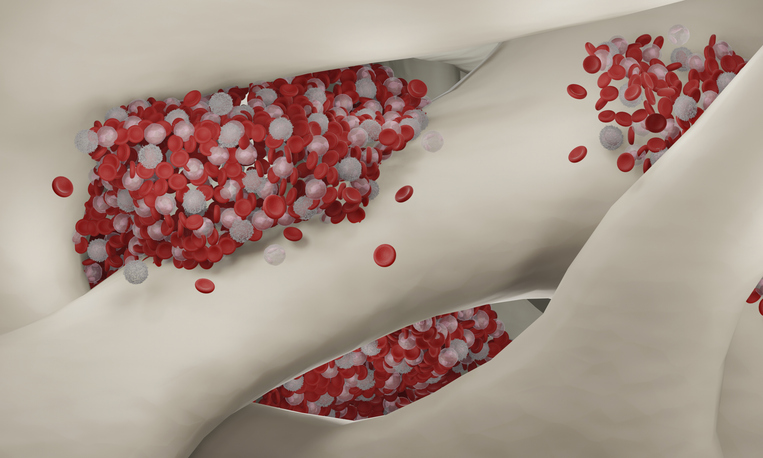
To investigate how non-small cell lung cancer (NSCLC) shapes immune response at the source, researchers used a combination of genetically engineered mouse models and samples from human NSCLC patients. Using single-cell transcriptomics and epigenomic profiling, they tracked the progression of myeloid progenitors in the bone marrow into tumor-infiltrating monocyte-derived macrophages (mo-macs).
In both human and murine systems, the researchers found early epigenetic reprogramming in granulocyte-monocyte progenitors (GMPs) and common monocyte progenitors (cMoPs), marked by increased chromatin accessibility in oxidative stress response genes and diminished interferon signaling pathways. These changes were sustained as the progenitors differentiated into TREM2hi and Arg1hi macrophages within the tumor.
These immunosuppressive macrophages, once embedded in the tumor microenvironment, exhibited high reactive oxygen species (ROS) levels, elevated expression of antioxidant genes like HMOX1, and reduced immune-stimulatory capacity. NRF2 activation, which was triggered in the bone marrow then reinforced in the tumor, played a central role in this transition.
This discovery has the potential to improve the performance of immunotherapies for NSCLC by targeting NRF2 and immune cells in the bone marrow to prevent it from initiating this immunosuppressive cycle. As Heged noted: “If we wait to target and rewire them until they’re inside the tumor, it may already be too late to reverse that process. We need strategies to intervene much earlier, while these cells are still developing, so we can stop them from becoming cancer’s allies in the first place.”
In mouse models, the team found that targeting NRF2 pharmacologically with inhibitors such as Brusatol and ML385, especially in combination with anti-PD-1 checkpoint inhibitors, improved tumor control. However, these effects were absent in NRF2-deficient mice, showing that NRF2 activity in myeloid cells is a key factor for creating an immunosuppressive tumor environment.
Using these findings, the researchers noted there is potential to develop blood-based diagnostics that can detect tumor-educated immune progenitor cells, to provide early detection of immune dysregulation in NSCLC. Therapeutic strategies could be developed to target NRF2 or its upstream signals—such as GM-CSF and IL-6, cytokines the researchers found are involved in the reprogramming process.
Another promising direction is the use of emerging drug modalities like targeted protein degraders (e.g., PROTACs or molecular glue degraders) to manipulate transcription factor activity in specific cell lineages. NRF2, as a regulator of stress responses, metabolism, and proteostasis, may serve as a nexus for controlling myeloid cell fate in malignancy.
The team will now explore whether NRF2-mediated progenitor cell reprogramming is a shared mechanism across other cancers and will look to better understand the broader metabolic and genetic networks involved in this process. They will also investigate extramedullary hematopoiesis and its relationship to tumor-driven immune remodeling.