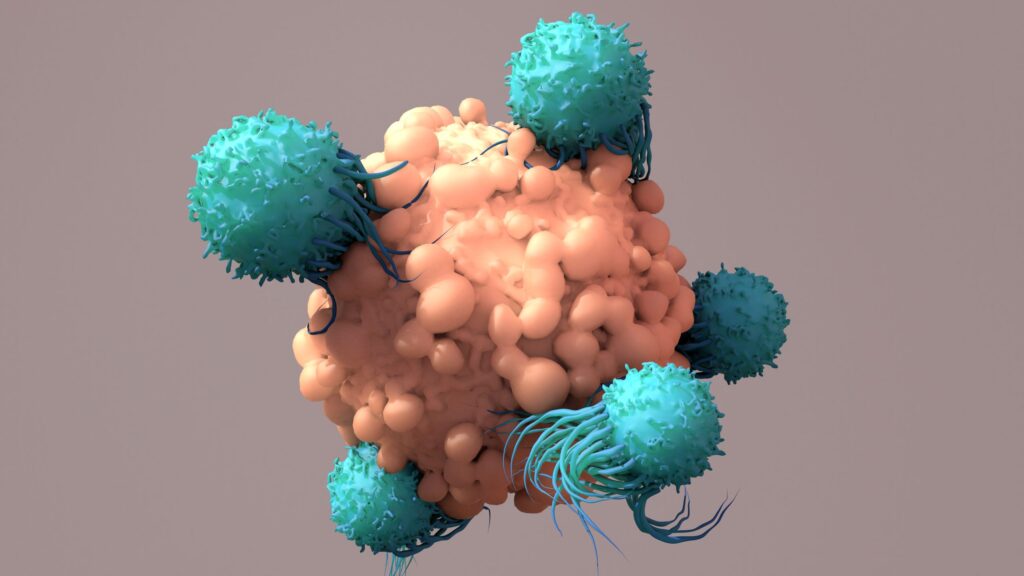
Cancer immunotherapy has historically focused on harnessing the ability of T cells to recognize and attack cancer cells. Adaptive immune checkpoint inhibitors (ICIs) unleash tumor-infiltrating lymphocytes (TILs) to fight cancer, offering cures to patients who have exhausted other treatment options. While tumors have a variety of strategies to develop ICI resistance, one of the key mechanisms is suppressing the recruitment of TILs. Turning immunologically “cold” tumors “hot” by activating innate immune recognition of cancer cells and recruiting TILs has been a longstanding goal of the immuno-oncology field.
In a new study published in Cell Reports Medicine titled “ENPP1 inhibitor with ultralong drug-target residence time as an innate immune checkpoint blockade cancer therapy,” researchers from the Arc Institute and Stanford University have developed an immunotherapy drug, STF-1623, which safely prevents cancer cells from hiding from the immune system’s first responders. The work was led by Lingyin Li, PhD, core investigator at the Arc Institute and professor at Stanford University.
The Li lab focuses on harnessing cGAMP, a second messenger molecule that activates the innate immune system by triggering the Stimulator of Interferon Genes (STING) pathway. ENPP1 is the dominant hydrolase of cGAMP and has emerged as a promising immunotherapy target. However, existing ENPP1 inhibitors have been optimized for prolonged systemic residence time rather than effective target inhibition within tumors. STF-1623 is a highly potent ENPP1 inhibitor with a long tumor residence time despite rapid systemic clearance, enabled by its high ENPP1 binding affinity and slow dissociation rate.
“This preclinical study represents the first successful tumor-specific targeting of an innate immune checkpoint, potentially offering a new approach for treating ‘cold’ tumors that don’t respond to current immunotherapies,” said Li. “We first synthesized STF-1623 in 2016. This research builds on years of work understanding how ENPP1 helps cancer cells evade the innate immune system and how we can restore its function.”
The surveillance protein, cGAS, detects the stray DNA from genomically unstable cancer cells and produces cGAMP in response. Cancer cells can disrupt this detection system by producing high levels of ENPP1. STF-1623 works by blocking ENPP1, allowing cGAMP to accumulate around cancer cells, enter surrounding immune cells, and trigger STING pathways to suppress cancer growth.
The STF-1623 mechanism differs from direct STING agonists, which have shown limited success in early clinical trials. Rather than artificially setting off the immune system’s most potent alarm, STF-1623 works by preserving naturally produced cGAMP in cancer cells, which potentially results in a more controlled and targeted immune response.
STF-1623 was shown to be effective in multiple mouse models of cancer, including breast, pancreatic, colorectal, and glioblastoma. No side effects were observed in mice, most likely because the drug only targets ENPP1 proteins highly concentrated in tumors and is quickly eliminated from the rest of the body.
Li predicts that these drugs will work best in concert with a patient’s treatment regimen, as STF-1623 was shown to be most effective in combination with other cancer therapies in rodent models. “Cancer is incredibly complex, and so, no single approach is likely to be sufficient for all patients,” she said. “What we’re trying to do here is help the body immunize itself against cancer by activating the innate immune system in the right place—at the tumor site.”