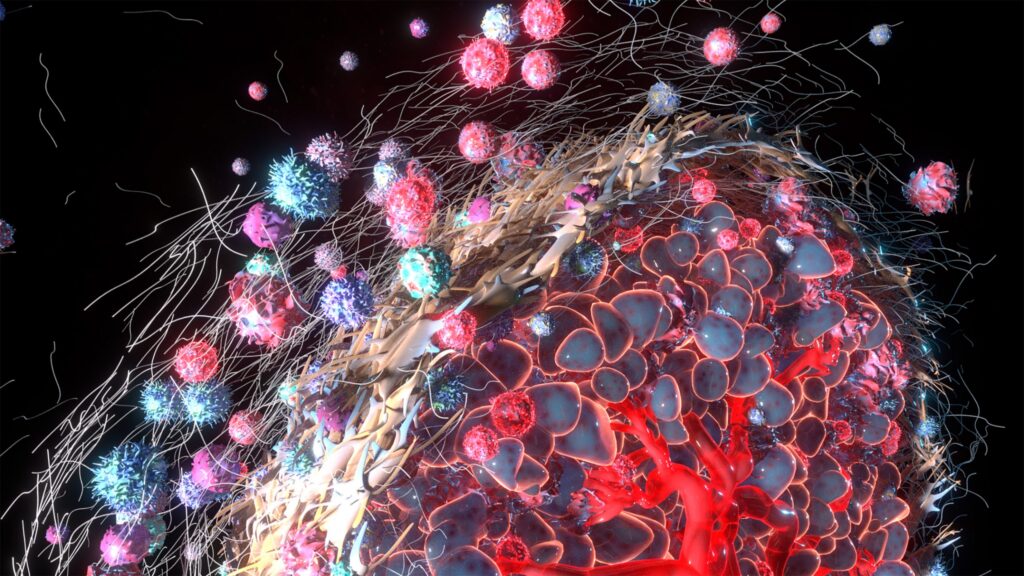
New research from the University of Pittsburgh shows that the low-oxygen and high acid levels of the tumor microenvironment (TME) put stress on mitochondria, creating events in these cellular energy producers that lead to T cell exhaustion. Their study, published in Immunity, shows that the toxicity of the TME results in mitochondria producing reactive oxygen species (ROS) that travel to a cell’s nucleus where it damages telomeres to produce a dysfunctional state in T cells.
“The really exciting part about this research is that by preventing damage to telomeres via a targeted antioxidant, we can rescue T cell function,” said lead author Dayana Rivadeneira, PhD, an assistant professor in the Pitt Department of Immunology and UPMC Hillman Cancer Center. “This opens the door to novel therapies to improve the effectiveness of cancer immunotherapies.”
In this new work, the research team didn’t initially look to study the role of telomeres. Instead, the initial focus was on mitochondrial dysfunction in T cells. But a collaboration with other Pitt colleagues helped them turn their attention to the role of damaged telomeres. To do this, the researchers developed mouse models with a genetic system that, when exposed to far-red light, generates targeted oxidative damage in either telomeres or mitochondria.
“What we found was remarkable,” said senior author Greg Delgoffe, PhD, a professor of immunology at UPMC Hillman. “Whether we damaged the mitochondria or the telomeres, we got the same result: dysfunctional T cells. There is crosstalk between the engine of the cell and the brains of the cell, the mitochondria and the nucleus. This is something we didn’t necessarily appreciate, at least in the immune system.”
The researchers detailed how the TME imposes both immunologic and metabolic stress on T cells, causing the accumulation of mitochondrial reactive oxygen species (ROS). These ROS travel to the nucleus and inflict DNA damage at telomeres.
Notably, this damage did not shorten telomeres which earlier research has shown links telomere attrition to senescence. The telomere dysfunction was evident through DNA damage markers such as ƔH2AX and 53BP1, indicating a fragile telomeric phenotype. This damage was enough to result in T cell dysfunction and resulting diminished capability for cytokine production, the researchers noted.
“When you damage the mitochondria, one of the first things that gets damaged is the telomeres,” Rivadeneira noted. “And, likewise, when you damage the telomeres, they talk back to the mitochondria to initiate a program that tells the cell to shut down and become exhausted.”
Looking for a method to prevent these affects on telomeres, the team applied a telomere-targeted version of the antioxidant GPX1, which they showed could prevent this damage. “Localizing the ROS scavenger GPX1 directly to telomeres reduced telomere fragility in tumors and improved the function of therapeutic T cells,” the researchers wrote. In mouse models with aggressive melanoma, animals treated with these modified T cells showed significantly smaller tumors and longer survival.
“This research is highly translatable because this approach could easily be incorporated into standard CAR-T protocol,” said Delgoffe. “While you’re genetically engineering T cells to improve cancer-fighting capability, you could also make them bulletproof against oxidative damage.”
The researchers are now developing a telomere-targeted antioxidant system suitable for use in human T cells, with an eye toward launching clinical trials to test this approach. Rivadeneira also plans to examine whether standard treatments like chemotherapy, which can damage DNA, also impairs T cell function by harming telomeres, potentially limiting a patient’s ability to respond to immunotherapy.
The research team also believe their finding may have implications beyond oncology to other conditions affected by a compromised immune systems such as chronic viral infections, inflammatory diseases, and aging.