Scientists from Mass General Brigham and the Broad Institute of MIT and Harvard have used CRISPR screens to identify genetic modifications that influence T cell function and survival in cultures and preclinical models of multiple myeloma. Their findings could be used to make chimeric antigen receptor T cell (CAR T) therapies more effective. Full details are provided in a new Nature paper titled “In vivo CRISPR screens identify modifiers of CAR-T cell function in myeloma.”
As the study’s co-senior author, Robert Manguso, PhD, a principal investigator in the Massachusetts General Hospital Cancer Center and director of the Tumor Immunotherapy Discovery Engine at the Broad, explained, the team performed a CRISPR screen over “the entire lifecycle of a T cell, co-culturing them with cancer cells, and then took the work a step further by transferring the cells to an animal model.” Those screens revealed “important regulators in vivo that we could not have predicted from the in vitro results.”
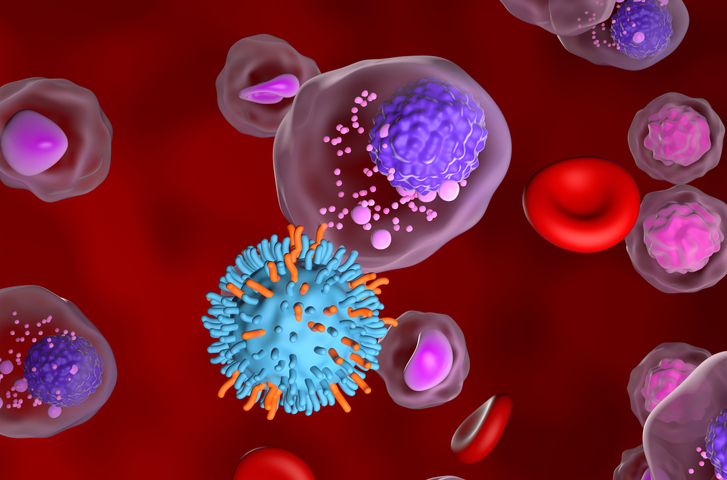
CAR T cell immunotherapies, which used modified T cells from patients, have been a boon for treating patients with blood cancers. However, they have not been as effective against solid tumors or in patients with relapsed or refractory multiple myeloma. In addition, the number of circulating CAR T cells decreases over time, which limits their long-term activity. Thus, strategies that improve the efficacy of these treatments could improve outcomes for a broader swathe of patients.
For the study, the research team developed a CRISPR screen that targeted 135 genes in human donor-derived CAR T cells to identify genes that could improve therapy persistence and function. They cultured the CRISPR-edited cells in vitro and then transferred them into a mouse model of multiple myeloma and tracked their survival in vivo for up to 21 days.
“Testing individual genetic modifications to find those that enhance CAR T function would take a huge amount of time and money,” said co-senior author Marcela Maus, MD, PhD, director of the cellular immunotherapy program at the Mass General Brigham and an associate member in the Broad’s cancer program. “Our approach lets us test hundreds of changes at a time.”
When the team analyzed the modified CAR T cells, the scientists discovered that deleting CDKN1B, a cell cycle regulator, increased CAR T cell proliferation, long-term persistence, and anti-tumor activity. Based on these findings, the authors believe that targeting CDKN1B in CAR T cells could enhance treatment outcomes for patients with multiple myeloma. Additionally, they suggest that future studies that harness their screening method could refine therapeutics for other cancers.
The data also showed that some genes affected function in vitro but not in vivo, while others boosted early proliferation in the tumor microenvironment but not long term benefits. Specifically, “ablation of RASA2 and SOCS1 enhanced T cell expansion in vitro, whereas loss of PTPN2, ZC3H12A, and RC3H1 conferred early growth advantages to CAR T cells in vivo,” the scientists wrote.