Every month, more than two billion people all around the world menstruate, generating a treasure trove of data that could indicate their health status. Yet, the sample containing this information—menstrual blood—ends up as waste.
“Some years ago, we realized that menstrual blood was a source of health information that was really underutilized,” said Lucas Dosnon, a graduate student in medical materials innovation researcher Inge Herrmann’s lab at ETH Zürich.
Lucas Dosnon, a graduate student in Inge Herrmann’s lab at ETH Zürich, helped design a smart pad that can detect disease biomarkers in menstrual blood.
Lucas Dosnon
Building on this, Herrmann, Dosnon, and their team developed a platform called MenstruAI, wherein wearable sensors embedded within a menstrual pad can detect disease-related molecules in menstrual blood.1 The sensors change color—which can be visualized directly or via a smartphone application—on coming into contact with disease biomarkers, signaling whether users need to visit the doctor. The researchers conducted a proof-of-concept study, published in Advance Science, which suggests that the platform could offer an accessible, non-invasive tool for tracking health among menstruators.
Menstrual Blood as a Window into One’s Health
In recent years, scientists identified that proteins and biomarkers in menstrual blood show a significant correlation with their concentration in venous blood. Researchers have used menstrual blood to monitor glycated hemoglobin levels in diabetic people, detect human papillomavirus which could cause cervical cancer, and identify endometriosis-related biomarkers.2-4

Inge Herrmann, a medical materials innovation researcher at ETH Zürich, developed a sanitary napkin that can detect disease-associated molecules in menstrual blood.
Inge Herrmann
So, when the idea to detect biomarkers in menstrual blood using a pad first struck Hermann, she brushed it aside. “I was like, probably someone has thought about that already,” she recalled. Digging into the literature offered some clarity: While researchers used dried blood spots on menstrual pads to study disease biomarkers, these methods required the blood to be eluted from pads and processed in laboratories.
Wanting to build something more user-friendly that did not require processing in the lab, Hermann looked deeper to see if such a tool existed. When none of her searches returned any results, she knew that her team was onto something.
Selecting Biomarkers and Creating the Pad
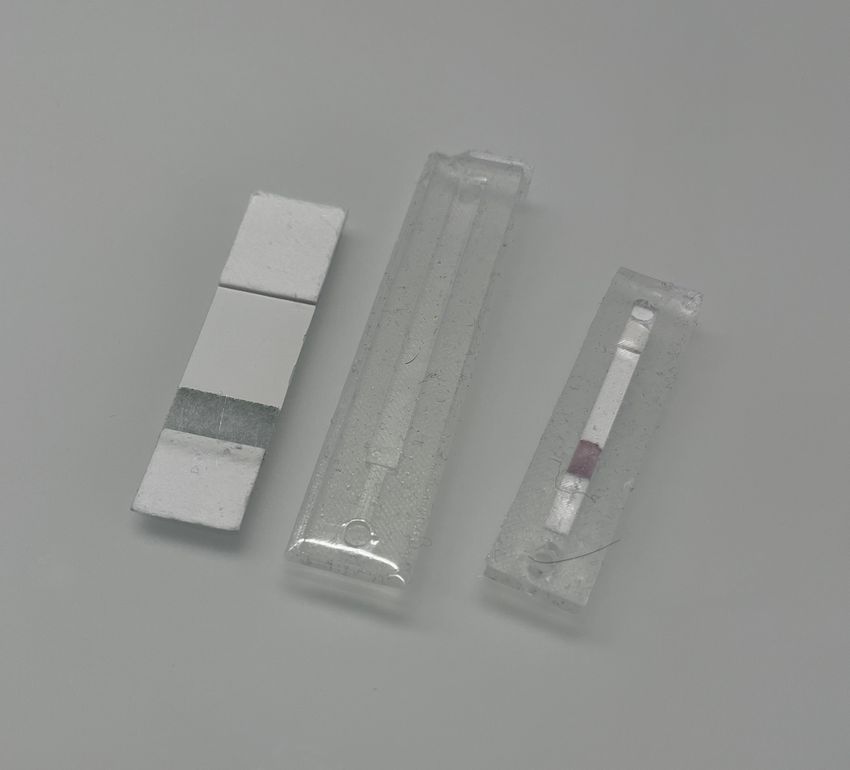
Elements composing MenstruAI’s sensor. From left to right, paper-based sensor platform from which single test strip can be cut, soft-silicon casing allowing integration of the paper-based sensor and blood flow control, and fully assembled sensor ready to be inserted into a sanitary pad.
Lucas Dosnon
To detect molecules in the menstrual blood, Herrmann, Dosnon, and their team designed a lateral flow assay-based test that follows the same principle as that of a home-based COVID-19 detection kit. The test strip, which contains antibodies, changes color when a particular molecule in the sample comes in contact with its specific antibody.
The researchers chose three biomarkers: C-reactive protein to signal inflammation, tumor-specific carcinoembryonic antigen for gynecological cancers, and cancer antigen-125 as an indicator of endometriosis and ovarian cancer. They optimized the sensors by adding venous blood containing known amounts of each biomarker on the sensors such that they would detect the molecules in a diagnostically-relevant range.
Then, the researchers focused on design strategies to embed these into a pad. They encased the sensors in a flexible, soft-silicon microfluidic casing equipped with an inlet that allows only a certain volume of blood to reach the device.
Proof-of-Concept and the Future of the Smart Pad
As a proof-of-concept, Herrmann, Dosnon and their team had volunteers collect their period blood in a menstrual cup. They spiked this with some biomarkers and validated that the device could detect them.

Christine Metz is a reproductive health researcher studying menstrual blood at the Feinstein Institutes for Medical Research.
Christine Metz
After integrating the sensors into pads, the scientists sought to test the pad’s comfort and functionality. They recruited volunteers to wear the pad during the second day of their period and go about their routines. In all the cases, the pad successfully collected the desired blood volume, leading to a complete lateral flow assay test. The volunteers reported no discomfort, noting that the prototype was as convenient as a commercially available menstrual pad.
Finally, to make result interpretation easier, the researchers developed a smartphone application. “Before disposing of [the pad, users] can take a picture of it, and the smartphone app will be here to help translate [the] results into clear insights,” said Dosnon. The application uses an AI-based algorithm trained on hundreds of test strip images to determine the concentration of different biomarkers and also enables sharing the results with healthcare professionals. They analyzed biomarker-spiked menstrual blood using this application and observed that it could reliably and accurately detect the molecules on par with detection in venous blood.
“This is very exciting,” said Christine Metz, a reproductive health researcher studying menstrual blood at the Feinstein Institutes for Medical Research, who was not involved in this research. “They have something that’s very simple to use. It’s an at home product, [and] it will be very inexpensive in its design.”
However, she noted that researchers do not fully understand the healthy range of biomarkers in menstrual blood for detecting complex diseases like endometriosis. “In menstrual effluent, we have no idea what any normal range of anything is,” she said. She also added that the biomarkers that Herrmann and her team tested for are not specific and may not be diagnostically relevant.

Integration of MenstruAI’s sensor inside a sanitary pad. The device is inserted below the first layer of the sanitary pad and can be pulled out after use.
Lucas Dosnon
Herrmann agreed that the biomarkers are not specific but noted that the pad is meant as a screening, rather than, diagnostic tool. “It’s basically a warning that maybe something’s off and should be checked by a doctor,” Dosnon added. “We are not trying to compete with traditional diagnostic methods.”
Metz added that she hopes that the researchers expand their project to include more people and provide another proof using menstrual blood tested directly on the pad rather than collected in a cup and poured over the sensors. Both Herrmann and Dosnon said that this is underway. They added that they are now working on a larger field study with more participants and testing for a larger panel of biomarkers.
Overall, Herrmann hopes that their work will inspire others to develop simple platforms to utilize the abundant information that menstrual blood has to offer.

