By exploring topics that at first seem unrelated to cancer, scientists have made therapeutic breakthroughs.
Cancer is one of the most common causes of death worldwide. But despite the countless hours that scientists have spent studying cancer and the billions of dollars that fund their efforts, for most cancers, a cure remains beyond grasp. Some researchers recently found inspiration in topics that may have seemed to have nothing to do with cancer. Learn about how their creative approaches may lead to therapeutic breakthroughs in this article.
Researchers recently discovered that they could treat high-grade glioma (HGG), an aggressive form of pediatric brain cancer, using avapritinib, a drug that gained FDA approval for gastrointestinal tumors. The team, led by Mariella Filbin, a pediatric neuro-oncologist and researcher at Dana-Farber Cancer Institute, found avapritinib when looking for drugs that were either approved or under investigation by the FDA and targeted platelet-derived growth factor receptor alpha (PDGFRA), a commonly mutated gene in HGG patients. When the researchers found that the drug could cross the blood-brain barrier in animal models, they thought that it would be a promising candidate for HGG. In collaboration with a biopharmaceutical company, Blueprint Medicines, the researchers conducted a small clinical trial involving eight patients with HGG, aged four to 29 years. They showed that the patients generally tolerated avapritinib well, and the drug even prolonged survival in three patients.
A drug that acts on a notoriously hard-to-target protein stabilized oral cancer progression and shrunk tumors in cats.
©iStock, Nils Jacobi
In a recent clinical trial involving 20 cats with oral cancer, Katherine Skorupski, a veterinary oncologist at the University of California, Davis, along with physician scientist Jennifer Grandis and biochemist Daniel Johnson at the University of California, San Francisco, investigated the safety of a drug against Signal Transducer and Activator of Transcription 3 (STAT3), a protein that is notoriously hard to target. The researchers discovered that the drug was not only non-toxic, but it could also shrink tumors and prolong survival in some cats. Since STAT3 is commonly hyperactivated in both human and cat cancers, and the drug targets a part of the protein that is 100 percent identical between cats and humans, the researchers hope that it may someday benefit human patients too.
Scientists once thought that dietary antioxidants, such as vitamin E, may potentially lower prostate cancer risk. But a large-scale study conducted by the National Cancer Institute in the early 2000s debunked this—revealing that vitamin E may instead increase prostate cancer risk. The unexpected finding motivated Lloyd Trotman, a molecular biologist at Cold Spring Harbor Laboratory, to investigate whether pro-oxidants, the opposite of antioxidants, could act as cancer drugs. Recently, Trotman and his team discovered that vitamin K precursors, specifically menadione sodium bisulfate, could promote prostate cancer cell death and as a result, prolong survival in mice, by increasing oxidative stress and depleting cells of lipids.

Carolyn Schutt Ibsen combines ultrasound-responsive biomaterials with tissue engineering to model tumors and develop novel therapies against cancer.
Noah Berger
Biomedical engineer Carolyn Schutt Ibsen of Oregon Health and Science University defines a fulfilling career as the ability to apply her training and skills in engineering to solve long-standing problems in cancer research. As a graduate student working in the laboratory of Sadik Esener, another biomedical engineer at Oregon Health and Science University, she optimized a method to deliver drugs using microscopic bubbles controlled by ultrasound. In this approach, scientists pack drugs or genes in lipid-coated bubbles, then apply ultrasound to burst the bubbles and disrupt cell membranes, allowing the cargo to enter cells. Driven by her passion for both engineering and cancer research, Schutt Ibsen now continues to explore this technology in her own lab. In 2024, the Biomedical Engineering Society’s Cellular and Molecular Biology group recognized Schutt Ibsen for her work in using bioprinted constructs for ultrasound-guided gene delivery.
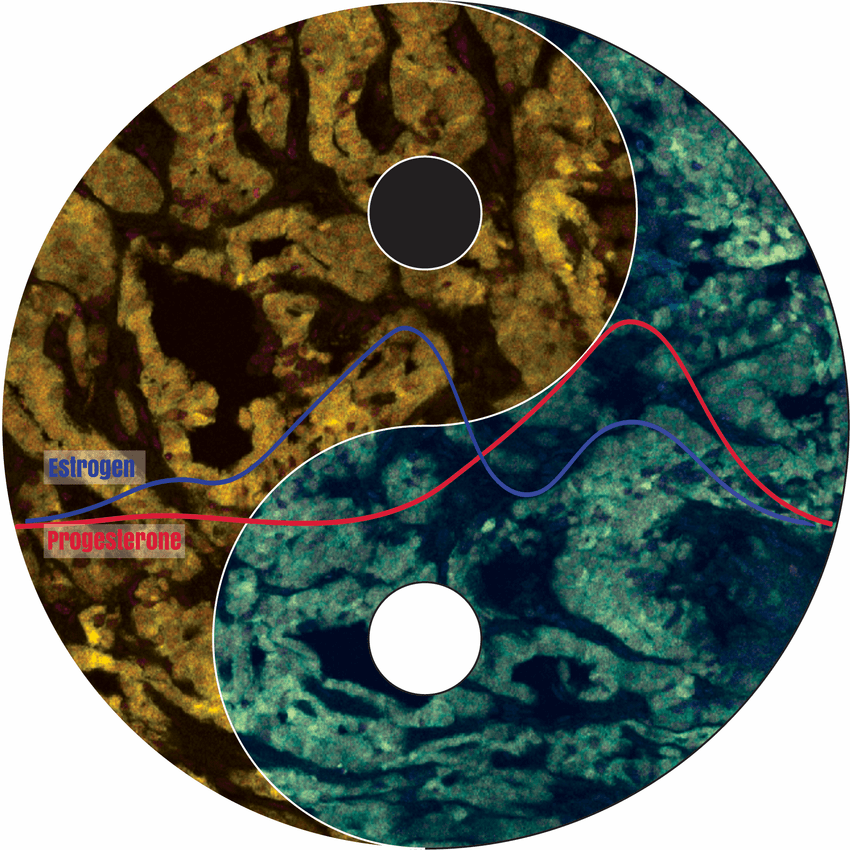
Ying and Yang: The menstrual cycle influences breast cancer and its response to treatment.
Laura Bornes, Netherlands Cancer Institute
When Colinda Scheele, a cancer biologist at VIB-KU Leuven Center for Cancer Biology, and her predominantly female team observed inconsistencies in the chemotherapy response of mice with breast cancer, they wondered if the menstrual cycle (called the estrous cycle) may be to blame. Recently, Scheele and her colleagues discovered that indeed, the menstrual cycle, affected the sensitivity of breast tumors to chemotherapy. The team observed that this was not only true for mice—they reached similar findings when analyzing data from human patients. This suggests that adjusting the timing of treatments to patients’ menstrual cycles may lead to better outcomes. While Scheele remains cautious about the translational implications of her findings, her team is currently designing a study to explore this possibility.

